4. Alternative and Natural Treatments
Often, traditional pain treatments like medications or surgery are ineffective. Some don’t touch the pain while others cause frustrating side effects. Fortunately, many alternative therapies offer viable options for treating your chronic pain. That’s why over half of Americans over 50 turn to these non-mainstream practices for help.
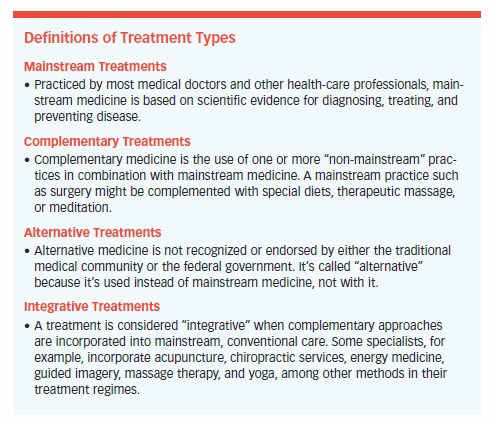
As for whether mainstream, complementary, alternative, or integrative medicine is best, the answer isn’t clear cut. What works for one person may be ineffective for another. Using complementary, alternative, and integrative treatments is a practice in trial-and-error. Effectiveness depends on multiple variables, including the person or team administering the treatment, the nature of the person’s condition, and the type of treatment being used. See “Definitions of Treatment Types,” on page 54.
Acupuncture
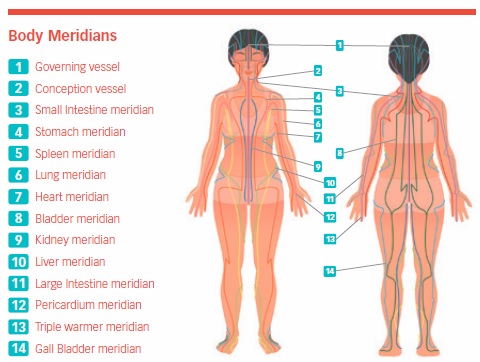
Acupuncture is an ancient Chinese technique that treats illness or provides local anesthesia by inserting needles for 10 to 30 minutes at specific sites on channels, or meridians, which correspond with internal organs. The effect, in theory, is to create a “life force,” or energy balance, to influence the progress of a disease or a condition, such as chronic pain.
Acupuncture is not recommended for people who are taking certain drugs or who are extremely anxious. It also is not appropriate for conditions such as head injuries, herniated discs, or unstable joints. A 2017 review of 29 trials involving 18,000 people concluded that acupuncture can enhance standard care by reducing the severity of chronic pain and depression.
Perhaps the strongest recent endorsement of complementary medicine, including acupuncture, was published in February 2017 when the American College of Physicians endorsed heat, massage, acupuncture, and spinal manipulation for the treatment of low back pain.
The National Center for Complementary and Integrative Health says that acupuncture appears to be a reasonable option for people with chronic pain. However, clinical practice guidelines are inconsistent in recommendations about acupuncture.
The National Institute of Neurological Disorders and Stroke states, “Medications, acupuncture, local electrical stimulation, and brain stimulation, as well as surgery, are some treatments for chronic pain.”
Studies have shown that acupuncture has varying degrees of effectiveness in treating fibromyalgia, knee osteoarthritis, tension and migraine headaches, lower back pain, and myofascial pain.
JAMA reported that acupuncture was associated with improved pain outcomes approximately half the time when compared to no treatment and sham (or “fake”) acupuncture. Sham acupuncture (which is used as a control in scientific studies) was successful in treating pain 42.5 percent of the time.
Studies in the United Kingdom and Korea found that there was “very little compelling evidence” that acupuncture reduced pain.
According to the American Academy of Orthopaedic Surgeons, acupuncture may help when combined with traditional pain-relief methods for:
- Low back pain
- Fibromyalgia
- Tennis elbow
- Stroke rehabilitation
- Osteoarthritis
- Muscle pain (knots)
- Carpal tunnel syndrome
If you decide to seek pain relief through acupuncture, get a recommendation for an acupuncturist who is certified by the American Academy of Medical Acupuncture (AAMA).
Electroacupuncture
Electroacupuncture delivers an electrical current through acupuncture needles to restore the flow of energy throughout the body. The needles used are half the thickness of those used to give injections and produce a sensation that feels more like an insect bite than a shot.
Treatment, which is most effective when used for 30 minutes, ranges from relatively painless to uncomfortable. Adverse side effects are rare, but may include bleeding, infection, and dizziness.
A study in the journal Anesthesiology found that electroacupuncture provides effective pain management when combined with low dosages of conventional analgesics.
The journal Lasers in Medical Science reported that laser acupuncture was effective in treating the pain associated with temporomandibular disorder.
Acupressure
With acupressure, stimulation is provided by touch rather than needles. When pressure is applied at specific points, it can (in theory) rebalance the body’s energy flow. Shiatsu is a Japanese form of acupressure.
A limited amount of evidence supports the practice of acupressure for pain control, relaxation, and stress management. One study showed that people with chronic low back pain who were treated with acupressure had an 89 percent greater reduction in disability compared to those in a physical therapy group. Two other studies showedlimited success using the practice to treat pain.
Aromatherapy
Aromatherapy is the use of essential oils from plants (by inhalation or bodily application) to improve the mind, body, and spirit, says the National Cancer Institute. This government agency has conducted or sponsored most of the current research on the topic. Essential oils are used by cancer people to improve their quality of life, reduce treatment side effects, and lower stress.
Aromatherapy may be used with other complementary treatments, such as massage and acupuncture. Among the oils used are those from Roman chamomile, geranium, lavender, tea tree, lemon, ginger, and cedarwood. They are thought to stimulate smell receptors, which send messages through the nervous system to the part of the brain that controls emotions.
Aromatherapy is used in three ways:
- Indirect inhalation (inhaled via a room diffuser, which spreads the oil through the air, or by placing drops of oil nearby.)
- Direct inhalation (breathed in through an individual inhaler.)
- Massage (massaged into the skin through lotions or bath salts.)
The FDA considers essential oils cosmetic, so manufacturers are not required to prove their product’s effectiveness, purity, or potency.
Studies of aromatherapy massage and inhalation show mixed results. Some reported improved mood, anxiety, sleep, nausea, and pain while others showed no change in symptoms.
The Mayo Clinic found that people who tried aromatherapy after surgery had better pain management and higher overall satisfaction with their care.
Another study suggested that lavender oil may help reduce pain for people with osteoarthritis of the knee.
A trial of 103 people with cancer found a decrease in anxiety and improved symptoms in a group that had massage with essential oil.
A 2016 review of several small studies published in Pain Research and Treatment indicated that aromatherapy can successfully treat pain when combined with conventional treatment.
Side effects are rare when essential oils are used according to directions, but can include allergic reactions, skin irritation, and sensitivity to sunlight.
Biofeedback
Biofeedback measures body functions related to emotional stress and chronic pain. Awareness of the physical changes that take place when a person’s under stress or feeling pain can help him or her manage those variables.
Electrodes placed on the body measure functions such as breathing and heart rate, blood pressure, skin temperature, and muscle tension. A monitor displays the results, which indicate which body function levels are abnormal. The person administering the biofeedback will then teach the person how to lower those indicators using techniques such as controlled breathing, imagery, and exercises.
The goal is to gain control over these body functions and, in the process, self-treat a variety of physical problems, including chronic pain.
Biofeedback has been shown to be ineffective at treating certain kinds of pain, including acute lower back pain. Also, there’s not enough evidence to suggest the technique is any more (or less) effective than any other pain-management method.
However, supplemental therapy that teaches pain coping and biofeedback skills together can reduce pain, the potential for pain, and health-care costs.
A 2017 study in the International Journal of Behavioral Medicine concluded that biofeedback treatment can lead to improvements on various pain-related, short- and long-term outcomes, both as a stand-alone and adjunctive intervention.
Copper Bracelets
While some strongly believe copper bracelets can relieve pain, no evidence exists to support their effectiveness. Manufacturers claim that tiny amounts of copper move through the surface of the skin and neutralize molecules that can damage cells in and around joints.
The most recent study on copper bracelets, published in PLOS ONE, found that wearing a magnetic wrist snap or copper bracelet did not appear to have any meaningful therapeutic effect beyond that of a placebo.
While copper bracelets and magnets aren’t harmful, studies suggest that they have value only as a placebo, easing pain in about 50 percent of people who use them.
Distraction
Distraction can be effective as a common sense, complementary treatment method for long-term pain, according to studies published during the past six years. Reading a book, talking with someone, listening to music, playing a game, or doing a crossword puzzle may reduce activity in the area of the brain that processes pain.
A study of 65 healthy undergraduate students published in The Journal of Pain found that creating mental space away from the pain can help reduce the discomfort you feel. (See “Distancing Yourself from Pain Can Lessen Discomfort.”)
Also, a study conducted at Columbia University showed that a combination of distraction and a placebo topical cream relieved pain. Listening to music can have a significant effect on chronic pain and depression. It also can make people feel more in control of their pain, less disabled by their condition, and distracted from their discomfort.
Another study showed that music incorporated into a pain-management program resulted in a 12 to 21 percent reduction in pain. Depression occurred 19 to 25 percent less in music groups than in control groups that did not use music as complementary pain therapy.
A study in Cyberpsychology, Behavior, and Social Networking found that people with chronic pain demonstrated significant pain relief while participating in virtual reality distraction activities.
A Current Biology study found that distraction is not just a psychological event, but an active, nervous-system mechanism reducing the amount of pain signals moving from the spinal cord to higher-order brain regions.
Joint Supplements
The only thing consistent about research on chondroitin and glucosamine is its inconsistency. The two supplements may be beneficial for certain populations, but the evidence is not conclusive and may never be.
If you and your doctor decide that either substance might be appropriate in treating your chronic pain, here are some factors to consider:
- The most commonly recommended dosages are 1,500 mg of glucosamine and 800 to 1,200 mg of
chondroitin daily (divided into two to three equal doses). - 30 to 90 days of use are needed to get an accurate assessment of their effectiveness.
- Use of glucosamine or chondroitin should be considered separately. The two substances are not automatically a combination-treatment strategy.
- No serious side effects have been reported, although one animal study found that chondroitin accelerated the growth of a type of melanoma (Molecular Cell 2018).
Hypnosis
Hypnosis has been described as a form of heightened concentration in which the person is unusually receptive to behavior-changing suggestions, either from the therapist or from something the person has written or recorded for later use.
Hypnosis can be directed by a therapist or by the individual in the form of self-hypnosis. The National Board for Certified Clinical Hypnotherapists (www.natboard.com) lists certified members by state.
Evidence suggests that self-hypnosis activates certain parts of the brain. Some think hypnosis may be able to change people’s expectations about the degree of pain, altering the whole pain experience thereafter. Others believe that hypnosis blocks the perception of pain by allowing a person to focus on an image. Advocates of therapeutic hypnosis agree that hypnosis puts a person into a deep state of relaxation.
The National Institutes of Health (NIH) and the American Psychology Association have endorsed hypnosis as a treatment for pain. A summary of studies showed that most people feel pain relief after receiving hypnotic suggestions. Other studies indicated that hypnosis is effective for relieving pain caused by cancer, irritable-bowel syndrome, and surgery.
Psychology Health has reported that hypnosis, biofeedback, relaxation therapy, and counseling all play roles in improving psychological outcomes and reducing pain.
Hypnosis doesn’t work for everyone—those who suffer from nerve damage are more likely to benefit from it than others.
Magnets
Magnet manufacturers claim their products are effective in treating fibromyalgia, back pain, headaches, neck, knee, and foot pain, but the scientific evidence to prove these claims is nonexistent.
“Scientific research does not support the use of static magnets for pain relief,” says the National Center for Complementary and Integrative Health.
Studies of magnet use in specific populations (degenerative knee pain, women with low back pain, and diabetics) have shown the treatment to be therapeutic. However, others have noticed no benefit. It may be that any positive results seen in studies are a result of the placebo effect. Any treatment is more likely to work if people believe that it will.
No research specifies how strong the magnets should be, how long they should be applied, whether they could be harmful, or exactly how they work.
Magnetic Stimulation
Repetitive transcranial magnetic stimulation (rTMS) is a non-invasive treatment that delivers magnetic pulses to the cortex of the brain. The FDA approved it in 2008 for the treatment of depression, and rTMS also has been used off-label to treat several disorders, including pain.
A 2017 study in Anesthesia Essays and Researches found that rTMS improved the efficacy of conventional medical treatment for chronic pain.
In 2015, Archives of Physical Medicine and Rehabilitation reviewed the effects of rTMS for chronic pain relief and concluded that rTMS has potential usefulness in the management of chronic pain. However, more studies on the different aspects of chronic pain are needed to provide a more solid basis for its clinical application.
The journal PAIN published a study in 2013 showing that rTMS is tolerable and provides modest relief among people with neuropathic pain. A Neurology study in 2014 found that rTMS improved symptoms of fibromyalgia.
Repetitive transcranial magnetic stimulation appears to be an emerging type of treatment for several types of chronic pain, but not one that the FDA has approved specifically for pain.
Massage
According to the American Massage Therapy Association, massage promotes health and wellbeing by way of soft tissue manipulation and movement of the body.
Studies claim that massage therapy may:
- Produce measurable changes in the body’s immune and endocrine response.
- Reduce the frequency of tension headaches, but not ease their intensity.
- Result in significantly less pain, anxiety, and depression among people with fibromyalgia.
- Reduce pain, improve function, and increase flexibility in people with knee osteoarthritis.
- Reduce pain in the short term, increase circulation, reduce muscle tension, and improve joint range of motion.
- Relieve symptoms without curing or reversing the course of any disease.
Multiple studies demonstrate massage’s effectiveness at reducing stress, pain, and muscle tension. However, evidence of massage’s ability to treat low back pain is mixed and inconclusive. A study of 104 people published in a 2017 issue of Pain Medicine suggested that massage might be helpful in treating low back pain.
Overall, evidence points toward beneficial effects for pain and symptoms associated with multiple conditions. These effects, however, are short term, meaning repeat massages are necessary to continuously notice positive results.
Engage in massage therapy with a positive attitude and with realistic expectations about what massage can and cannot do for you.
Marijuana
According to the National Conference of State Legislatures, 34 states, the District of Columbia, Guam, Puerto Rico, and the US Virgin Islands have approved medical marijuana programs. And 12 states allow the use of “low THC, high cannabidiol (CBD) products for medical reasons.”
While many people believe in marijuana’s ability to combat a number of medical conditions (depression, anxiety, glaucoma, AIDS wasting syndrome, neuropathic pain, cancer, multiple sclerosis, chemotherapy-induced nausea, and certain seizure disorders), some of the research is compelling.
Many who try marijuana hope to manage their pain without the nasty side effects associated with other medications such as opioids, and many are doing so without a prescription. While some medical professionals worry about a patient’s desire to self-medicate with marijuana, most see this drug as a more favorable option than the opiates.
Medical marijuana is administered as an oil, pill, vaporized liquid, nasal spray, dried leaves and buds, and the plant itself.
Many of the effects of marijuana, whether medical or recreational, are the result of the active ingredient called delta-9-tetrahydrocannabinol (THC), which resembles a chemical produced naturally by the body and brain. THC is an FDA-approved medication for nausea associated with cancer chemotherapy and for stimulating appetite in people with severe weight loss that often accompanies AIDS. Cannabidiol (CBD) is another component of marijuana that may have analgesic effects.
Recent Findings
Seniors in states with approved medical cannabis laws take less pain medications (including opioids), found a study published in JAMA Network in May 2018. According to researchers, prescriptions filled for all opioids under Medicare Part D (used primarily by seniors) decreased by 2.1 million daily doses once a state instituted a medical cannabis law and by 3.7 million daily doses when medical cannabis dispensaries were opened.
A 2018 study published in the European Journal of Internal Medicine found that cannabis therapy was safe and effective for several pain-causing conditions, including cancer pain. Researchers also found that medical cannabis treatment significantly relieved pain and improved the quality of life for seniors with minimal side effects.
As of May 2019, the FDA had “not approved marijuana as a safe and effective drug for any indication.” It has, however, approved the synthetic form of cannabidiol (CBD), Epidiolex, for use in treating seizures from Lennox-Gastaut syndrome or Dravet syndrome.
Meditation
If practiced properly, meditation can banish stress and anxiety, improve sleep, and relieve chronic pain in many. Those practicing the concentration model of meditation silently or quietly repeat a word, sound, or thought, “the object of attention,” as the focus of their attention. When extraneous thoughts or feelings (like pain) enter your thoughts, your focus should be returned to the object of attention.
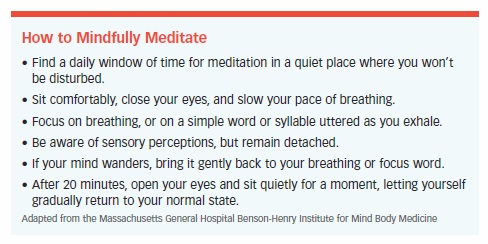
Those who practice mindfulness meditation focus on a single thought or process (like breathing) and slowly expand their awareness to include thoughts, feelings, and sensations other than pain.
Meditation takes discipline and practice—it’s not easy to shut out distractions. Learn a few pointers in “How to Mindfully Meditate.”
Recent Findings
JAMA Internal Medicine reported that mindfulness meditation programs “can help reduce severe pain and increase function for older adults with chronic low back pain.”
A study conducted in Denmark found that mindfulness meditation led to lower anxiety and depression, better quality of life, and feeling in control of pain.
University of North Carolina scientists found that training in meditation practices for three days produced relaxed states and reduced pain when a group of subjects were exposed to painful stimuli.
Researchers at Wake Forest University showed that meditation reduced pain intensity by 40 percent as a result of less activity in the area of the brain normally associated with pain.
The Journal of Pain reported that meditation might be an effective treatment for reducing chronic neck pain.
Other studies have indicated that mediating can reduce stress, relax muscles, slow breathing, reduce episodes of depression, enhance immune response, and diminish awareness of pain.
Platelet-Rich Plasma
Platelet-rich plasma (PRP) is a component of a person’s own blood that has a platelet count concentrated five to 10 times higher than normal—blood plasma enriched with platelets.
PRP is derived by taking a small amount of the person’s blood and using a centrifuge (a rapidly rotating container) to separate the platelets. The concentrated platelets and plasma are then injected into the injured area. This procedure has the potential to speed healing and repair a variety of soft-tissue injuries.
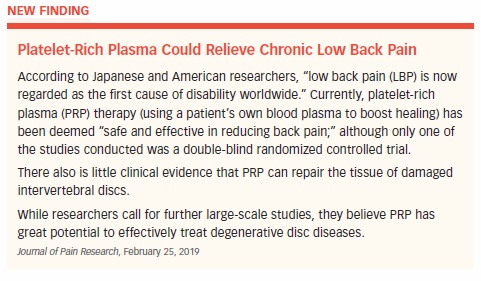
Many people are so excited about PRP that they’re rushing to use it despite inconclusive evidence about its efficacy for specific injuries or conditions.
Although PRP appears to be effective in treating chronic elbow injuries, the medical community needs more scientific evidence before it can determine whether PRP will be successful for other conditions, says the American Academy of Orthopaedic Surgeons.
In January 2017, one study provided an optimistic projection for using PRP to treat knee osteoarthritis.
The Hospital for Special Surgery says there is limited support of PRP treatment in published clinical studies. Since PRP is created from a person’s own blood, however, it’s considered relatively low risk with a potential to improve or speed healing.
Since the FDA has yet to regulate its use, some physicians who use PRP to treat certain soft-tissue injuries are doing so “off label”—they’re prescribing PRP for a purpose other than the one it’s being used for.
Prolotherapy
Also referred to as proliferation therapy, prolotherapy is an injection-based procedure. Considered safe for most, it involves injecting a watery substance including dextrose, saline, or sarapin and a numbing agent (lidocaine) into the affected area. This triggers the body’s healing process, encouraging it to regrow healthy ligaments and tendon fibers.
Prolotherapy has been used for multiple conditions, including injuries to the joints and connective tissues of the neck, knee, shoulder, hip, pelvic floor, hands, and lower back.
Recent Findings
Evidence is mixed. A study in Cochrane Review found no proof that prolotherapy was effective for chronic low back pain. And one of the nation’s largest insurers considers prolotherapy “investigational and not medically necessary” for all conditions involving joints and ligaments.
However, prolotherapy combined with spinal manipulation, exercise, and other therapies has provided good results for lower back pain. Prolotherapy for chronic shoulder pain caused by tendinitis also is effective, according to some studies.
Researchers at the University of Wisconsin reported that a series of injections containing dextrose and sodium resulted in less pain, reduced stiffness, and greater knee function among people with osteoarthritis.
A systematic review of dextrose prolotherapy for chronic musculoskeletal pain supported its use in treating knee and finger joint OA and spinal/pelvic pain due to ligament dysfunction, according to a study published in Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders.
The take home: While prolotherapy might be effective for certain conditions in some people, the evidence is inconclusive.
Stem Cell Therapy
Also known as regenerative medicine, stem cell therapy involves three steps:
- Growing stem cells in a lab.
- Developing these into cells corresponding to those in various parts of the body.
- Implanting the cells into damaged tissues.
The FDA says stem cells have the potential to repair, restore, replace, and regenerate cells, and could be used to treat many medical conditions and diseases. However, the agency is concerned that some people seeking cures and remedies are vulnerable to stem cell treatments that are illegal and potentially harmful.
A 2017 review study in Pain Physician sums up the current status of stem cell research regarding pain: “Though the data from existing studies look promising for the use of stem cells as a strategy for discogenic pain, neuropathic pain, and osteoarthritis, additional studies will be needed to validate the benefit of the technology for clinical use.”
Tai Chi
A low-impact exercise highly recommended for those in chronic pain, tai chi lacks conclusive evidence to prove that it’s helpful.
Tai chi combines relaxation, meditation, and deep breathing with slow, gentle, continuous, and structured exercises called forms, including: “standing, graceful postures,” “achieving harmony between body and mind,” and “meditation in motion.”
The number of movements in tai chi varies from 18 to more than 100. A beginner can start learning with a five-minute weekly session and work up to a target goal. Tai chi is especially effective in older adults because it can be practiced at different intensity levels.
The NCCIH offers a cautiously optimistic summary of tai chi research. Evidence-based studies suggest that practicing tai chi may improve balance and stability in older people and those with Parkinson’s, reduce pain from knee osteoarthritis, and help people cope with fibromyalgia and back pain.
Indirectly, exercise of any kind seems to reduce pain, so tai chi qualifies in that respect. Some evidence shows that tai chi reduces the amount of stress hormones produced, and general anecdotal evidence suggests that tai chi reduces stress.
Small studies have shown that tai chi may help people with fibromyalgia, shingles, and knee osteoarthritis.
For most, tai chi appears to be a safe, body-friendly activity. However, anyone who has acute chest pain with minimal exertion, severe shortness of breath, dizziness, fainting spells, or uncontrolled blood pressure should seek a doctor’s advice before starting tai chi, as should those with osteoporosis, acute back pain, or active infections.
Yoga
More than 36 million Americans practice yoga, says the Yoga Alliance’s 2016 Yoga in America Study. Of these participants, 72 percent are women. The practice of yoga, which uses movement, meditation, relaxation, and gentle breathing, contributes to a sense of relaxation and self-awareness.
The American Pain Foundation calls yoga “an ancient method of stilling the mind.” For some, yoga is more spiritual. For others, it’s an alternative exercise promoting flexibility, strength, and endurance. Some use yoga to escape depression, or to calm their nerves and thereby ease chronic pain.
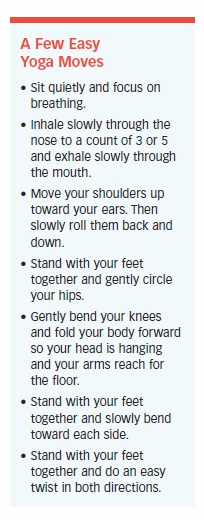
Yoga has a few essential components including:
- The “contraction and release” principle, which involves holding (and then releasing) certain postures/poses. This purportedly dissolves physical and emotional barriers, allowing energy to move to areas of chronic pain.
- Specific breathing exercises, which are thought to elevate mood and calm the central nervous system.
Yoga doesn’t have to be practiced in a yoga studio or gym. Instead, take breaks to breathe deeply and add “A Few Easy Yoga Moves” to your day.
Under certain conditions, yoga has been shown to relieve pain caused by carpal tunnel syndrome, headaches, fibromyalgia, and osteoarthritis of the hands. Studies regarding the health benefits of yoga include:
- Chronic pain: A presentation at the American Pain Society showed that yoga and meditation can counteract the effects of chronic pain.
- Fibromyalgia: At Arizona State University, yoga-type slow-breathing techniques reduced pain intensity in groups of healthy women and among women with fibromyalgia.
- Pain, disability, depression: A study funded by the NCCIH found that people who practice yoga had significantly less disability, pain, and depression.
- Pain, morning stiffness, physical function, depression: Studies reviewed in the Journal of Evidence-Based Complementary and Alternative Medicine showed that yoga reduced pain and morning stiffness, improved physical function, and was associated with lower levels of depression among people with osteoarthritis.
- Back pain: The Journal of Family Practice reported that people who performed yoga experienced an improvement in back pain symptoms. In Archives of Internal Medicine, yoga and stretching were found to be equal in reducing low back pain.
- Migraine headaches: The journal Headache found that yoga, in combination with breathing techniques, relaxation exercises, and meditation, reduced the frequency and intensity of migraine headaches.
The post 4. Alternative and Natural Treatments appeared first on University Health News.
Read Original Article: 4. Alternative and Natural Treatments »

