2. The Origins of Pain
A whopping 50 million American adults suffer from chronic or severe pain. According to data from the 2012 National Health Interview Survey, 25 million of these cases are chronic.
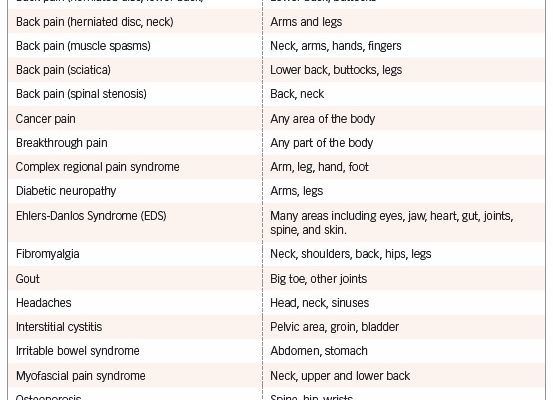
Chronic pain may be caused by an injury that begins, of course, as acute pain, but then is either so severe or long-lasting that the nerves are permanently damaged. The pain feels more intense and becomes chronic (see “Pain-Causing Conditions and the Areas They Affect”).
For many others, chronic pain can be blamed on one (or more) of the following:
- According to the American Academy of Family Physicians, conditions that may trigger chronic pain include infections, headaches or migraines, back problems, cancer, arthritis, fibromyalgia, nerve damage, and previous surgery.
- Surgery. Estimates vary, but up to 20 percent of back surgeries can fail, leaving continuous pain.
- An unknown reason. In some cases of chronic pain, doctors fail to pinpoint a definite cause.
The first step in gaining control of your pain is education. This chapter explains the many common causes of chronic pain, including the most commonly reported joint disorder (osteoarthritis) and the most debilitating (rheumatoid arthritis). Once you are familiar with what’s causing the hurt, you can learn how to relieve it.
Arthritis
Responsible for causing pain and stiffness in the joints and bone, osteoarthritis (OA) affects 30 million Americans. It’s the most common form of arthritis. Rheumatoid arthritis (RA), which affects about 1.3 million, is the most debilitating form of arthritis. RA is an autoimmune disorder that is chronic and progressive. It causes inflamed joints, painful deformity and often immobility (especially in the wrists, fingers, ankles, and feet).
Osteoarthritis
Also called degenerative joint disease, osteoarthritis is the result of worn joint cartilage and underlying bone. Before age 45, the condition is more common in men; after that, it’s more prevalent in women. By 75, more than 80 percent of Americans either have symptoms or x-ray evidence of OA. Half of people over 65 show evidence of the condition in at least one joint. Nearly half of all Americans will develop knee osteoarthritis during their lifetime.
When you have OA, the cartilage—the cushion in joints that protects the ends of the bones—thins, so the bones rub against each other. The result is pain, inflammation, swelling, and limited movement. The body tries to heal the damage, but it’s not very effective. In the worst cases, bone spurs develop, which are new bone that further worsens the pain and limited movement.
Those at highest risk of OA are obese, have a previous joint injury, or have a family history of the disease. A 2017 study found that weight loss can slow the degeneration of knee joints.
Symptoms. The symptoms of OA depend on which part of the body is affected, but can include:
- Stiffness
- Swelling
- Pain
- Difficulty bending and moving
- Restricted range of motion
Hip OA: Osteoarthritis in the hips causes pain, stiffness, and severe disability. Activities such as moving and bending become limited, making even a simple act like getting dressed a challenge. Those with the condition can feel pain in their hips, groin, buttocks, or knees.
Knee OA: A study published in Arthritis Care & Research found that knee pain when using stairs may be one of the earliest symptoms of knee osteoarthritis.
Spinal OA: Spinal osteoarthritis causes stiffness and pain in the neck or lower back, as well as weakness or numbness in the arms and legs.
Treatment. Treatment for OA includes weight control, rest, medications, alternative therapies, braces, joint injections, surgery, and exercise. Researchers from the University of Melbourne found that increasing knee extensor (quadricep) strength helped relieve OA pain and improved physical function.
In some cases, joint-replacement surgery (arthroplasty) is required. This involves removing damaged joint surfaces and replacing them with plastic or metal parts. Procedures are most commonly performed on the knee and hip joints.
Rheumatoid Arthritis
RA is an immune-mediated inflammatory disease that attacks the lining of the joints. The exact cause of RA is not known but genetic, environmental, and hormonal factors (in women) are implicated.
RA progresses through three stages: 1) swelling in the lining of the joints, 2) rapid division and growth of cells that cause the lining to thicken, and 3) inflamed cells that release enzymes. The enzymes digest bone and cartilage, which causes joints to lose their shape and alignment, both of which affect movement.
Symptoms include:
- Inflammation in the wrist and finger joints closest to the hand
- Fatigue
- Fever
- Feeling unwell
- Pain or stiffness for more than 30 minutes in the morning or after a long rest
- Tender, warm, swollen joints
- Same joint affected on both sides of the body (both wrists, for example)
- Symptoms that last for years
Limit Damage. The earlier you treat rheumatoid arthritis, the less damage you’ll experience. Treatment focuses on minimizing damage, controlling pain, lifestyle changes (joint protection, diet, and exercise), and reducing inflammation through a combination of drugs that usually includes methotrexate, an immune suppressive drug.
A modified-release form of prednisone appears to be more effective at reducing morning joint stiffness than the standard version of the steroid. The drug tofacitinib citrate (Xeljanz) may be used to treat moderate-to-severe rheumatoid arthritis in people who haven’t responded to or can’t tolerate methotrexate.
Disease-modifying arthritis drugs (DMARDs), although effective, aren’t reaching those who need them most. DMARDs aren’t pain-relieving medications. They’re designed to slow the progression of joint damage. Despite their possible success, at least two-thirds of older people aren’t getting these medications because of cost or the reluctance of primary-care physicians to prescribe them due to possible side effects and complications. The oral medication baricitinib (Olumiant), which received FDA approval in 2018, provides a new option for some RA people who don’t respond to current treatments.
Injections, physical therapy, exercise, and surgery are other treatment options. Changes in symptoms and health status must be monitored closely (at least every two to four months) and treatment changed accordingly.
Back Pain
Eighty percent of us will have back pain at some point, most often in our lower backs, but usually it will get better, with or without treatment.
The back’s muscles, bones, joints, ligaments, tendons, and discs must work together in perfect harmony to avoid injuries Even healthy people can suffer from back problems.
No case of back pain is the same. The causes, symptoms, and treatments of back problems vary, meaning they shouldn’t be treated as a single condition.
Lower Back Pain
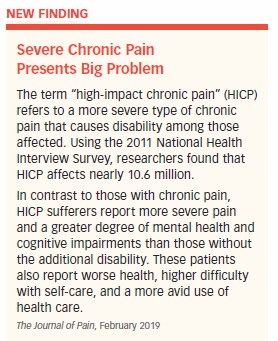
Lower back pain is the most common cause of disability. In 2018, researchers at the National Institute on Aging and Johns Hopkins University studied 878 aging adults to determine the effects of lower back pain. They found that 31 percent of people had mild low back pain and 16 percent experienced it as moderate-to-severe pain. While gait speed wasn’t affected, pain resulted in greater energy needed to walk and a poor perception of endurance. A worse perception of walking ability is likely to lead to loss of future mobility.
Lower back and/or leg pain are common symptoms of a herniated disc. A disc is like a soft, jelly donut. It sits between the vertebra to make up your spine. When a disc “slips” or becomes “herniated” or “ruptured,” its soft “jelly” middle bit squishes out through a tear in its exterior. The result is usually weakness, numbness, and tingling that radiates from the buttocks to the toes, and often pain.
The pain worsens with walking, standing, and during any activity that causes intra-abdominal pressure, such as coughing, sneezing, or straining with a bowel movement. Muscle weakness can occur in the affected leg, and muscle spasms are common. The pain resolves with or without treatment in up to a third of all cases, but the process can take weeks.
How a Back Strain Happens
The most common back injury is a strain or pulled muscle. Considering the long-term problems associated with other types of back problems, a pulled muscle is by far the least serious, even though at first it feels as bad as the others.
Back strains usually occur after sudden or awkward movements, when lifting or moving a hefty object, or absorbing a heavy or unexpected blow. Even something as small as bending down to tie a shoe can cause a strain.
Structural problems may cause low back pain and accompany strains. A bulging disc (the soft material between vertebrae) may press against a nerve. If the nerve extends downward through the leg, it can cause a shooting pain called sciatica, affecting the buttocks and back of the leg.
The lower back is one of the most frequent areas affected by osteoarthritis. Other structural problems, such as sciatica, herniated disc, and spinal stenosis, are discussed later.
Symptoms include pain and back spasms. If the pain is intense, you need immediate medical treatment, especially if it spreads down one or both legs, causes weakness or numbness, or follows a fall or blow to the back.
Treatment includes:
- Rest your back for 24 to 48 hours; limited, mild movement is better than complete bed rest.
- Apply ice packs for 15 to 20 minutes, three to four times a day for the first 48 to 72 hours.
- Apply moist heat after the first 48 to 72 hours if it feels more comfortable.
- Acetaminophen may relieve pain. Aspirin, ibuprofen, and naproxen may reduce both pain and inflammation. Check with a doctor if you have liver, kidney, or stomach problems before taking these medications.
- Side sleepers: Place a pillow between your knees.
- Back sleepers: Place a pillow under your knees.
Most pain medications have little-to-no effect on back pain. As a result, doctors suggest alternatives such as heat, massage, yoga, spinal manipulation, and acupuncture, claim Australian researchers.
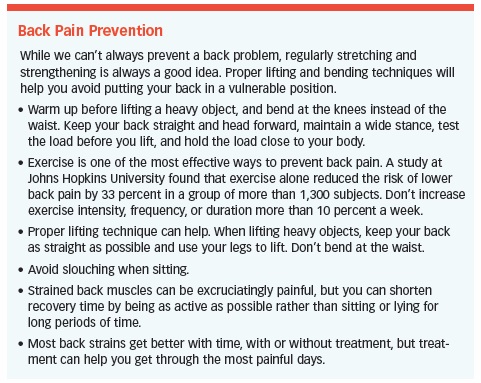
If you start feeling better, don’t overdo it. Avoid sitting in one position for long periods of time. Get up and stretch every 20 to 25 minutes. Slowly and carefully execute each movement required in daily activities before trying to do them in real time and real situations. (See “Back Pain Prevention,” on page 19.)
Facet Joint Syndrome
Facet joints allow the back or neck to extend and rotate from side to side. When the joints are inflamed, movement becomes restricted, leading to pain and a limited range of motion.
While the cause of facet joint inflammation isn’t always known, trauma, degeneration, and osteoarthritis are often blamed. The condition is more likely to occur in the upper part of the spinal column than in the lower back but can develop in either area.
The inflamed site can be sensitive to pressure because the capsule of the facet joints contains sensory nerves. Severe pain occurs when the surrounding muscles become involved. If the dysfunctional facets lie between the shoulder blades, the pain can radiate up to the shoulders and neck.
Treatment options include brief rest, joint immobilization, anti-inflammatory drugs, muscle relaxants, and exercises. Injections also are used. These affect the joint and/or block the associated nerves. For some people, facet nerve ablation can provide longer relief.
Herniated Disc
A herniated disc is a tear in the fibrous ring of tissue surrounding the disc. Some of the soft gelatinous material inside breaks up, bulges into the spinal canal, and may put pressure on a nerve. Anyone can develop a herniated disc, but older adults are especially susceptible.
A bulging disc (as opposed to a herniated disc) has been described as like having low air in a tire. Some of the cushion in the middle of the ring is lost, the disc collapses, and the fibrous ring bulges out. A bulging disc is a normal phenomenon and generally does not cause symptoms, except when it presses on the nerve roots.
A herniated disc is caused by wear and tear on the spine and often manifests after a simple activity, such as bending over, heavy lifting, or any strenuous activities that generates abdominal pressure. That pressure is transmitted to the disc, often in the L4/L5 vertebrae area. Prolonged sitting and repetitive lifting and twisting are risk factors, as is reduced muscle tone caused by a lack of physical activity.
Treat Symptoms at Home
Before heading to the doctor for a herniated disc, try using rest, ice, and anti-inflammatory pain medications. Apply ice for the first 48 to 72 hours before switching to moist heat. Get back to mild activity (like slow, easy walking) as soon as possible. Increasing evidence proves that mild movement is more effective than complete or extended periods of bed rest. If that doesn’t help, you need to see a doctor.
Long-term treatment under a physician’s care includes physical therapy, medications, and epidural steroid injections. Epidural steroid injections deliver steroid medications around the compressed or irritated nerve root. This technique is effective in improving pain and functionality, as well as decreasing disability. It might, in special cases, save people from having unnecessary surgery. Transcutaneous electrical nerve stimulation (TENS) devices, which are available over the counter, send electrical impulses into the area and can reduce pain in some people.
A new technique still at the research phase suggests that tissue engineering, in the form of harvesting and reintroducing the body’s own stem cells, may be a promising way to treat herniated discs in the lower back.
Surgery Candidates
If the disc won’t heal, there’s loss of bowel or bladder function or progressive leg or foot weakness, you may need surgery. Whether you have surgery or not, there’s a five percent risk of the condition recurring and a greater risk of future back pain.
Neck Pain
A herniated disc in the neck is a degenerative condition, sometimes confused with pain from bone spurs or arthritis. In most cases, no specific event triggers the herniated disc.
Symptoms include:
- Neck pain
- Slowed arm reflexes
- Numbness
- Tingling
- Weakness
- Pain that radiates down the arm
Treatment
Elevating the affected arm, bending the elbow, and placing the hand behind the head often relieves pain. This maneuver eases the pressure on the nerve and enlarges the opening through which the nerve exits the spine. Immediate treatment includes rest, NSAIDs, and physical therapy. A heating pad may help relieve muscle spasms.
Long-term relief comes through the use of a heating pad, prescription pain relievers, and physical therapy, which may include traction. A physician may prescribe a systematic series of exercises developed specifically for this type of problem.
Surgery is reserved for spinal-cord compromise, persistent arm pain or progressive arm weakness. When it’s required, the procedure involves removing the disc (discectomy), or a fragment of the disc (microdiscectomy), and fusing the adjacent spinal levels.
Muscle Spasms
Back spasms happen for a variety of reasons. Injury to the muscles, tendons, and ligaments (i.e. back strain) are one cause. More serious medical conditions such as arthritis or a bulging disc also can trigger surrounding muscles to involuntarily contract. The weaker your abdominal muscles, the more prone you are to back spasm. Having tight hamstrings and weak lower back muscles also puts you at higher risk.
There’s no mistaking a back spasm. Its sharp, sudden pain is triggered by an involuntary muscle contraction, often in the lower back. Its pain can be incapacitating. For relief from a spasm try these steps:
➧ Get into a less painful position. Lay on a firm surface, either on your back or side, with a pillow between your knees to take the edge off.
➧ Move. Limited, gentle movement is better than total bed rest. Once the pain becomes tolerable, try walking slowly for a few minutes several times a day.
➧ Apply an ice pack for 15 to 20 minutes, three to four times a day for the first 48 to 72 hours. Cold dulls the pain and may reduce inflammation. You may also use moist heat to increase circulation and make you more comfortable. Or, alternate ice and heat applications. Whatever makes you feel better is the way to go.
Pain relievers like aspirin, acetaminophen (Tylenol), ibuprofen (Advil, Motrin), and naproxen (Aleve) can alleviate pain and reduce inflammation.
If the spasms won’t stop, call your doctor. He or she may want you to come in and may prescribe one of several muscle relaxants, such as cyclobenzaprine (Flexeril), methocarbamol (Robaxin), or carisoprodol (Soma). Spinal manipulation is one of several options that can provide mild-to-moderate relief from low back pain and spasms.
Preventing Back Spasm
Avoid sitting in one position for long periods of time. Stand up and stretch every 20 to 25 minutes. Slowly and carefully practice each movement required during a normal day (i.e. sitting, reaching). Use a lower back support to remind you to evenly distribute pressure on the muscles of the lower back.
When lifting heavy objects, keep your back as straight as possible and use your legs to lift without bending at the waist.
Losing a few pounds will relieve stress on the muscles prone to spasm. Regular physical activity that includes strengthening exercises will help you move more easily and safely. Examples are wall squats, knees to chest, trunk raises, and leg lifts.
Sciatica
Pain that shoots from your lower back through your buttocks and down your leg, possibly into your feet is likely sciatica. Most commonly caused by a herniated disc in the lower back, symptoms can be mild or severe. They range from numbness and tingling to that shooting pain we mentioned.
In rare cases, sciatica causes the loss of bladder or bowel control. If this happens, it’s an emergency that may require surgery. The symptoms may be worse when you cough, sneeze, sit, or do certain types of exercise.
Risk factors for sciatica include:
- Age (30 and over)
- Frequently twisting the back
- Genetic factors
- Diabetes
- An occupation that involves excessive bending, lifting, or driving for long periods of time
- Smoking
- Excess weight
A study of more than 5,000 people found quitting smoking helped reduce back pain in people being treated for spinal problems. The reason, as other studies have shown, is that nicotine increases pain.
Ways to prevent sciatica include, good posture, stretching, walking, swimming, lifting objects safely, sleeping on the back or side, and avoiding sitting or standing for long periods of time.
Spinal surgeons usually recommend a short period of rest followed by exercises to improve flexibility, mobility, and strength in the back. Working with a physical therapist can help chronic pain caused by sciatica. Your doctor also may recommend hot and cold applications. Analgesic and anti-inflammatory drugs, such as naproxen, ibuprofen, and aspirin can dull pain and reduce inflammation.
Spinal Stenosis
Stenosis is a condition in which the spinal canal narrows and puts pressure on the spinal column or nerves. This narrowing may be due to a herniated disc that encroaches on the spinal canal from the front or thickened ligaments in the rear, or even enlarged arthritic facet joints that encroach on the canal from the sides.
A small number of people are born with shortened spinal structures called pedicles, which can lead to symptoms of spinal stenosis at a relatively young age. Stenosis occurs most often in the lower back (75 percent of the time); less often in the neck.
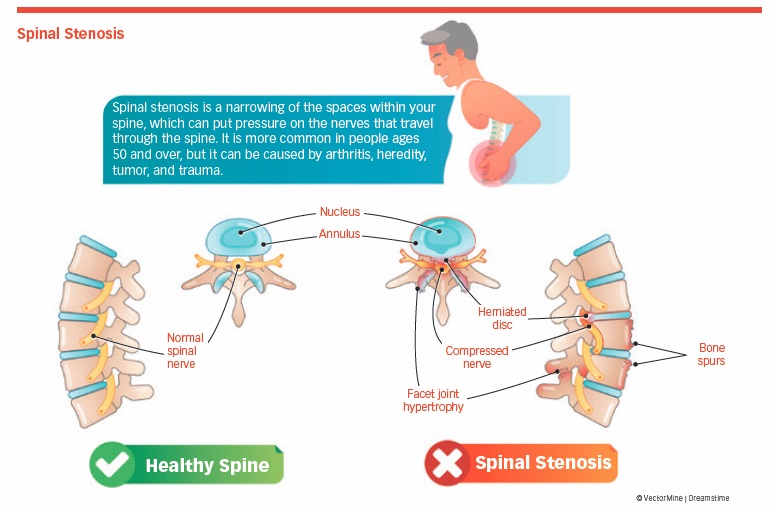
Spinal stenosis is commonly caused by aging (it’s more prominent in those over 50), arthritis, heredity, tumors, trauma, and repeated back surgery. Symptoms include pain in the lower back and legs that can be aggravated by walking and standing. The size of the spinal canal decreases significantly in the erect position (standing and walking) but returns to normal size when sitting or bending forward.
Symptoms include:
- Low back pain
- Numbness, tingling
- Hot or cold sensation
- Weakness
- Leg fatigue with prolonged standing or walking
- Feeling of clumsiness
- Falls
Finding Relief
Lean forward slightly while walking or lying down with your knees drawn to your chest. This position can help relieve pain in the short-term. For more long-term relief, try anti-inflammatory medicines, such as aspirin and ibuprofen, and rest the affected area.
In some cases, epidural steroid injections may be recommended. Unfortunately, they’re no panacea. They don’t provide long-term relief in moderate-to-severe cases.
Minimally invasive spine surgery can effectively treat spinal conditions, including stenosis, herniated disc, and sciatica. This involves smaller incisions, less loss of blood, and faster recovery. Success rates vary greatly.
Breakthrough Pain
Breakthrough pain (BTP) is defined by the American Cancer Society as a flare of pain that occurs even though the person is regularly taking medicine for chronic cancer-related pain.
BTP episodes are unpredictable, may occur more frequently when the person is engaged in a specific activity (incident pain), and may happen toward the end of a dosage period of persistent-pain medication. Pain “flares” vary in length, but peak intensity usually occurs in as little as three minutes and lasts an average of 30 minutes, according to pain specialists at the University of Pennsylvania.
The recommended treatment for BTP is a strong, short-acting opioid medication that works quickly. BTP medication is taken on an as-needed basis as soon as symptoms are experienced.
Cancer-Related Pain
Cancer pain can be caused by the disease, its treatment (including chemotherapy or radiation therapy), or both. Between 30 and 50 percent of people with cancer experience pain caused by the treatment, and 70 to 90 percent of those with advanced-stage cancer report pain from the disease itself.
Tumors may put pressure on organs, bones, or nerves, and they can obstruct the bowels or the flow of blood. The chemotherapy, radiation, and surgery used to treat cancer produce side effects, which can include discomfort.
Cancer pain develops when nerve endings detect damage in the body. The pain signal travels through nerve pathways to the brain, which interprets the message as pain. In some cases, the nerve pathways themselves have been damaged.
Cancer pain should be managed. About 85 to 90 percent of people with cancer and chronic pain can control their pain successfully. Both chronic pain and episodes of acute pain can be eased with medications. That said, 10 to 15 percent of people with cancer may require aggressive interventions or surgery to control their pain.
CRPS
Complex regional pain syndrome (CRPS) is a chronic neurological condition that most commonly affects one limb (i.e. an arm, hand, leg, or foot). This usually occurs after an injury. CRPS is one of the least understood forms of chronic pain, affecting women at twice the rate of men. One study found that siblings of people with CRPS and under the age of 50 were at three times higher risk of developing the condition.
There are two types of CRPS: Type I results from irritation of the peripheral and central nervous system without evidence of nerve damage. The condition might be precipitated by major or minor injury, trauma, or surgery. Type II has the added complication of peripheral nerve damage.
Pain that’s disproportionate to the severity of the initial event might be due to CRPS. It gets worse over time, and the pain can spread to the entire arm or leg. Possible symptoms include:
- Intense, burning pain
- Skin sensitivity
- Swelling
- Sweating
- Color changes in the affected area
- Increased skin temperature in early cases; decreased temperature in advanced cases
- Atrophy and loss of limb function (in late stages)
Treatment
There’s no specific diagnostic test for CRPS, nor is there a cure. The goal of treatment is to rehabilitate the affected limb to avoid loss of function, while trying to control symptoms. Analgesics, antidepressants, corticosteroids, opioids, nerve blocks, spinal or peripheral nerve stimulation, and drug-infusion pumps are a few treatment options. These measures give temporary relief in some people, but the response is unpredictable.
Spinal-cord stimulation provides substantial long-lasting relief to a good percentage of CRPS people for whom other therapies fail to relieve symptoms. Physical therapy and nerve blocks are other treatment options.
No single treatment will produce a long-lasting solution in every person, although CRPS goes into remission in some people. The best outcome is achieved if this condition is treated as early as possible.
According to the National Institute of Neurological Disorders and Stroke, immunoglobulin administered intravenously, low doses of an anesthetic agent called ketamine, and hyperbaric oxygen therapy are emerging treatments for CRPS.
Diabetic Neuropathy
Diabetic neuropathy is a nerve disorder associated with diabetes—specifically with elevated blood sugar levels that are characteristic of the condition. Although arms and legs are most likely to be affected, the damaged nerves can affect different areas of the body, including the brain, retina, heart, kidneys, bladder, stomach, and intestines.
Although DPN is a disease of the peripheral nerve, it appears that changes within the central nervous system also are related to the development of both painful and painless DPN.
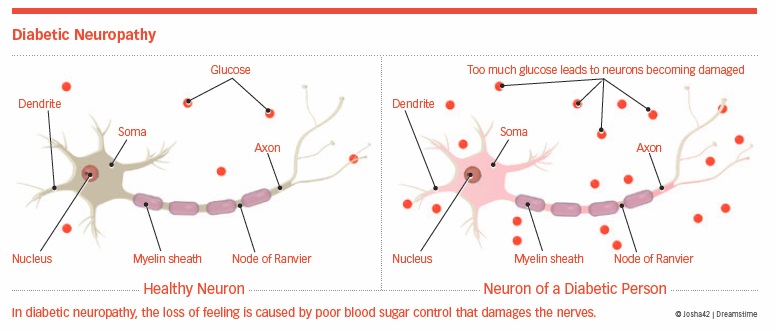
When peripheral nerves are affected, the condition is called peripheral neuropathy. Diabetic neuropathy is related to the duration of the diabetes, which cannot be controlled, and to poor blood sugar control, which can (and should) be controlled.
Between 60 and 70 percent of diabetics eventually will develop some form of neuropathy. The risk increases with age, the amount of time a person has had the disease, and poor control of blood-sugar levels.
In diabetic neuropathy, a loss of sensation is caused by damaged nerves.
DPN is most likely caused by several factors, including high blood glucose and fat levels, low levels of insulin, damage to blood vessels, autoimmune factors, mechanical injury to nerves, inherited traits, and lifestyle choices, such as alcohol use and smoking. Symptoms include:
- Tingling or burning sensation in the arms and legs
- Unaware of stepping on a sharp object
- Unaware of blisters or cuts
- Insensitive to hot or cold
Diabetic neuropathy is diagnosed with a physical exam, electromyogram, computed tomography (CT) scan, magnetic resonance imaging (MRI), and/or nerve-conduction velocity tests.
Diet, exercise, and medications, such as pregabalin (Lyrica), duloxetine (Cymbalta), and other anti-seizure drugs are effective. Duloxetine is normally used to treat depression, incontinence, and certain types of pain, but a review of 18 trials and more than 6,000 people found that it’s also useful in treating diabetic neuropathy.
Spinal cord stimulation (SCS) has emerged as a treatment for DPN. A study of 49 people found that SCS was successful in reducing chronic pain symptoms up to five years after beginning treatment.
The prognosis for DPN people depends on how the diabetes is being managed, says the National Institute of Neurological Disorders and Stroke. Treating diabetes may stop the progression and improve symptoms, but recovery can be slow.
Ehlers-Danlos Syndrome
Ehlers-Danlos syndrome (EDS) is the name for a group of 13 inherited disorders that affect connective tissues (collagen, in particular). Think of these tissues as a form of glue. They provide strength and support to our skin, bones, blood vessels, and other organs. They also support the tissues (i.e., ligaments, cartilage, and tendons) in and around our joints.
In a person with EDS, the connective tissues are extremely loose, meaning they don’t hold things as stable as they should, leaving them able to stretch far beyond the normal range. The result: frequent dislocations, subluxations (partial dislocations), torn ligaments and tendons, chronic pain, fatigue, instability and, sometimes, life-threatening complications such as the rupture of large arteries (in severe forms).
Those suffering from EDS most often present with soft, stretchy, easily-bruised skin, hypermobile joints, and poor wound-healing. While symptoms overlap for the various types, it would be extremely rare for a person to suffer from more than one form of the condition.
Diagnosis and Treatment
Diagnosing EDS isn’t easy. “Although there is a wealth of information easily accessible, it can still take a very long time [often more than 20 years] before the penny drops and someone recognizes the diagnosis and points the individual in the right directions for help,” says Dr. Alan J. Hakim, a London-based rheumatologist and EDS expert.
“Even then, there can be reluctance among some—family members and medical personnel alike—to acknowledge the syndrome, the depth and breadth of its insult, and the psychosocial impact on an individual’s well-being,” says Dr. Hakim.
There is no cure for EDS. Physical therapy, targeted exercises, and pain relief medication can help manage symptoms.
Fibromyalgia
Fibromyalgia is a chronic disorder with extensive symptoms, including areas of the body that are especially sensitive and painful to pressure or touch. The exact cause of fibromyalgia is unknown, but some studies show that genetic factors may predispose certain individuals to the condition. The pain from fibromyalgia is real. It’s more common in women than in men and usually develops between the ages of 35 and 60.
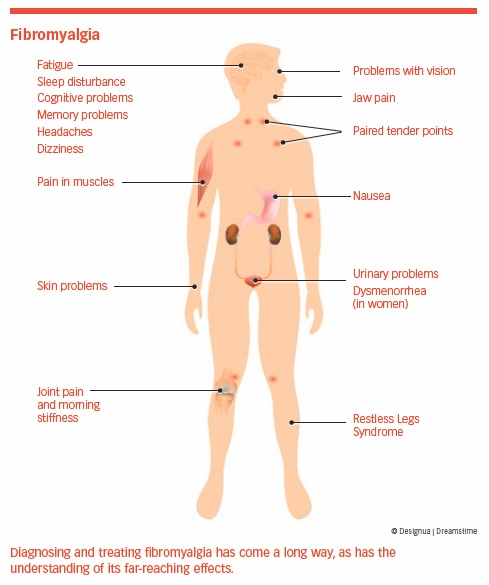
Fibromyalgia is characterized by widespread muscle pain and multiple tender points on the neck, shoulders, back, hips, and extremities. More than 75 percent of people report chronic fatigue as a major symptom and impairment, according to the Johns Hopkins Arthritis Center.
The tender spots vary in severity from one day to another. At times, they can be more severe in the shoulders; at others, more severe in the lower back and legs. Pain can interfere with sleep.
Most people are diagnosed during middle age, but symptoms can develop earlier. Fibromyalgia can cause pain and fatigue, but doesn’t inflame or damage joints, muscles, or other tissues. Other symptoms of fibromyalgia include:
- Headaches
- Irritable bowel syndrome
- Memory problems
- Morning stiffness
- Sleep disturbances
- Restless legs syndrome
- Numbness or tingling in the extremities
- Painful menstrual periods
- Temperature sensitivity
- Depression
- Dizziness
Causes
According to recent research, fibromyalgia is related to how the body processes pain and its hypersensitivity to factors that don’t normally cause discomfort.
A small study published in Scientific Reports in January 2018 found that hyperactive brain networks could play a part in the hypersensitivity experienced by fibromyalgia people. Known as explosive synchronization (ES), this condition can lead to a small stimulus causing a dramatic and synchronized reaction to the brain’s network. The researchers concluded that “the chronic pain brain is electrically unstable and sensitive.”
Those with rheumatoid arthritis, lupus, and spinal arthritis are more likely to develop fibromyalgia than people without these conditions. Fibromyalgia also has been associated with physically or emotionally stressful events, such as car accidents, repetitive-use injuries, and illnesses.
Treatment
People typically see several doctors before getting a diagnosis. Once the condition is identified, a team approach (doctor, pharmacist, physical therapist, and other specialists) works best. Three medications are FDA-approved for fibromyalgia: duloxetine (Cymbalta), milnacipran (Savella), and pregabalin (Lyrica). Other drugs prescribed by doctors include analgesics and antidepressants.
A Queen’s University scientist found that combining pregabalin (an anti-seizure drug) with duloxetine (an antidepressant) could improve pain relief, physical function, and overall quality of life in fibromyalgia people, according to the journal Pain.
Nonsteroidal anti-inflammatory drugs, such as ibuprofen, aspirin, and naproxen, are not particularly effective in treating fibromyalgia when taken alone, says the American Academy of Family Physicians (AAFP).
Complementary and alternative therapies, such as massage, chiropractic, acupuncture, and dietary supplements, produce varying degrees of success in treating fibromyalgia. Getting adequate, quality sleep can improve the symptoms of pain and fatigue, and an increasing body of evidence suggests that exercise is an effective treatment.
It’s important to be active with your care. Follow your doctor’s recommendations, make lifestyle changes that will help you feel better, and focus on short-term, realistic goals.
Among the lifestyle changes is an increase in moderate, low impact, planned exercise. Recognize stress and take steps to deal with it (see Chapter 1). Follow a daily routine that includes going to bed, getting up, and eating at regularly scheduled times.
No one treatment plan is effective for everyone. You know how you feel, what you can and cannot do, and how fibromyalgia is affecting your life. Work with your pain-management team to develop a strategy that fits your situation.
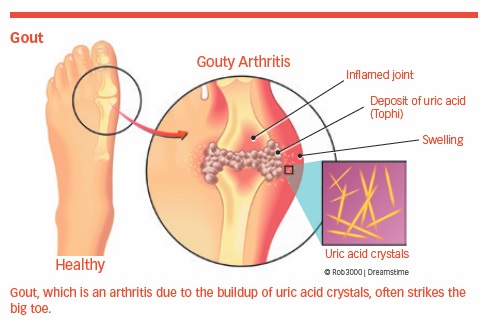
Gout
A disease caused by excessive amounts of uric acid and the needle-like crystal deposits left behind, gout is a form of arthritis. The excess uric acid may be due to the body producing too much of it or because the kidneys cannot efficiently remove it from the body.
Affecting more than 8 million Americans, this condition commonly affects the small bones of the feet but also can attack other parts of the body. Relatively few of those affected take measures to avoid the next flare-up, which can be both sudden and severe.
Two recent studies showed that a proper diet and medications could delay, minimize, or even prevent an attack by addressing the causes of gout rather than only its symptoms.
Eat Well
A diet recommended by the National Heart, Lung, and Blood Institute to address hypertension may be part of the solution in dealing with gout. A BMJ study found that the DASH diet (Dietary Approaches to Stop Hypertension) is associated with a lower risk of gout. Researchers used food frequency questionnaires of more than 44,000 men to classify those who followed a DASH diet and those who chose a predominantly Western diet.
A DASH diet is high in vegetables, nuts, legumes, low-fat dairy products, and whole grains. In contrast, the typical Western diet has a high intake of red and processed meats, fried foods, refined grains, as well as sweets and desserts.
Men in both groups were monitored for 26 years to determine the incidence of gout. The DASH diet was associated with a significantly lower risk, suggesting that its effect of lowering uric acid levels translated into a lower risk of gout. The Western diet was linked with a higher risk.
Risk factors in addition to diet include the use of alcohol, gender (men are more likely to have gout than women), age (30 to 50 for the first bout), being overweight (body mass index over 25), and race (African men twice as likely to report gout than Caucasian men).
Treatment
Although gout is recognized as a chronic disease, many doctors and patients treat it as an acute condition. In November 2017, the AAFP issued a position statement based on more than 8,000 patient medical records that stated managing gout with medications and treating it as a chronic condition could help prevent recurrences and associated repeat doctor visits.
Two medications that prevent the production of uric acid are allopurinol (Zyloprim) and febuxostat (Uloric). Allopurinol was approved by the FDA in 1966, but in 2017 the agency approved a combination of allopurinol and lesinurad (Zurampic) for gout-associated hyperuricemia, which is an abnormally high level of uric acid.
A disconnect has existed between available evidence regarding the treatment of gout and putting that evidence into practice. If patients closely follow DASH diet guidelines while physicians are more proactive in treating gout as a chronic condition, flare-ups would decline dramatically.
Headaches
Tension headaches, migraines, cluster, sinus, hormone, acute, exertion, and caffeine headaches—there are at least 30 types of headaches, and the location of the headache offers an indication of its type. (See “Headache Primer.”)
Headaches can be on one side (unilateral) or both sides (bilateral). Some may be intermittent, episodic, or constant while others are acute—they come and go rapidly. Still others persist for days or weeks. When the exact location of the pain can’t be identified, it’s called a generalized headache.
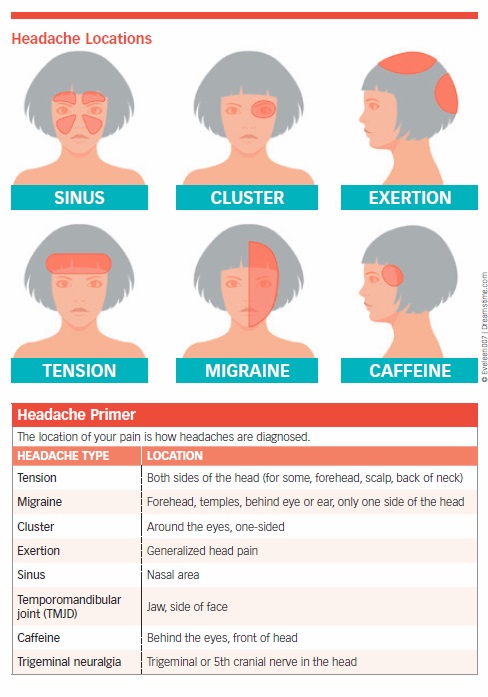
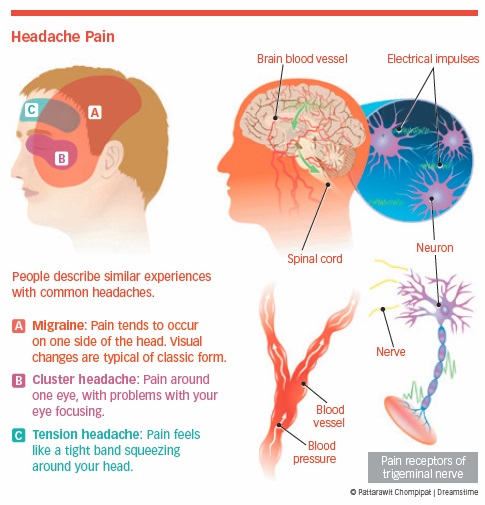
Cluster Headaches
Cluster headaches are one of the most painful types. They cause excruciating pain on one side of the head, around the eyes, and sometimes affect the nose and other areas of the face. They’re called cluster headaches because they occur daily (in clusters). These headaches come on suddenly and can last from 15 minutes to three hours. They’re more common in men and can go into remission for months or years.
Exertion Headaches
Exertion (activity-related) headaches are triggered by physical activity, especially lengthy exercise sessions. They usually develop at the height of exercise and subside when the activity stops, although some can last up to two days.
Exertion headaches are more common in adolescents and adults up to age 50. Most often, they’re harmless, but you can’t make that assumption. See your doctor to rule out underlying serious causes.
Sinus Headaches
Sinus headaches often are caused by a cold, sinus inflammation, allergies, and other respiratory infections. The distinguishing characteristic is deep, constant pressure-like pain in the cheekbones, forehead, or bridge of the nose. This can worsen with sudden head movement or straining, and can be accompanied by fever, runny nose, and clogged ears.
Caffeine Withdrawal Headaches
Unless you’re drinking about 500 mg of caffeine per day (i.e. four to five cups of coffee), you probably won’t have a caffeine-withdrawal headache. If you are drinking that much and suddenly stop, you’re likely to experience one. The problem is temporary, although it may take a few days to return to normal. The solution is simple: Consume less caffeine and reduce intake slowly.
Tension Headaches
Two types of headaches—tension and migraine—are associated with chronic pain (see “Is It a Tension Headache or a Migraine?”).
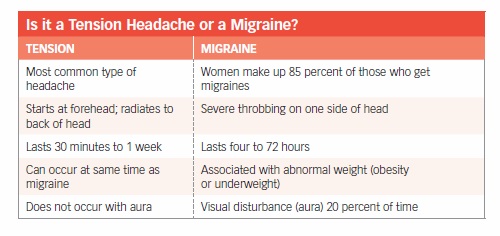
Tension headaches aren’t accompanied by other symptoms and are usually triggered by fatigue or stress. People who have them describe a feeling of pressure on both sides of the head. Others experience pain that involves the forehead, scalp, or back of the neck. Tension headaches can be mild, moderate, or severe, but aren’t usually debilitating. However, occasional episodes can develop into chronic, long-term pain.
Tension headaches can be caused by contractions of the muscles in the head and neck, and expanded blood vessels in the scalp can contribute to the discomfort. The headaches can be triggered by any number of factors, including an argument with a spouse, traffic, job pressures, working at a computer for long periods of time, and poor posture. Arthritis of the cervical facet joints also might be a cause. A lack of exercise appears to be associated with non-migraine headaches.
These headaches are usually treated with over-the-counter drugs such as aspirin, acetaminophen, or ibuprofen. If you’re experiencing them for more than 15 days a month, you have chronic pain and should see a doctor. He or she might prescribe antidepressants, blood-pressure medication, or anti-seizure pills.
Migraines
A migraine involves recurring episodes (two or more a month) of head pain, plus sensitivity to light and sound. Nausea, vomiting, and neck pain can accompany the discomfort. Ten to 20 percent of the time the person who is about to experience a migraine gets a warning, called an aura. An aura may be a tingling sensation or visual distortion (seeing zigzag lines) that lasts from 10 to 30 minutes.
Migraine headaches are a neurological disorder. Treatment methods are being developed to target peripheral and central nervous systems. Migraines are often misdiagnosed as sinus headaches because pain also is across the forehead and the bridge of the nose.
Triggers. The exact mechanism that causes migraines is not fully understood. Current thinking focuses changes in blood flow and the excitability of brain cells. Though it’s difficult to pinpoint a cause, triggers include:
- Hormonal changes (caused by menstrual periods or estrogen)
- Diet (particularly alcohol, chocolate, monosodium glutamate, caffeine, or marinated foods)
- Bright lights
- Strong odors
- Stress
- Fatigue
- Poor sleep patterns
- Biochemical processes in the brain
- Vascular disease
- Weight (A 2017 study published in Neurology found a 27 percent higher risk with obesity and a 13 percent higher risk in those who are underweight)
Daily fluctuations of variables such as weather, diet, hormone levels, sleep, and stress make it difficult to pinpoint a reason without clinical testing.
Treatment. A physician might suggest changes in sleep or eating habits and will probably prescribe medicines to block the pain. Medications called triptans can prevent or treat a migraine. These include sumatriptan (Imitrex), eletriptan (Relpax), and rizatriptan (Maxalt). Injectable triptans have an 80 percent success rate; triptan tablets are 60 to 70 percent effective in treating migraines. Antidepressants and drugs used to treat high blood pressure (including beta-blockers) can be preventative.
Injecting an anesthetic or onabotulinumtoxinA (Botox) directly into tender muscles in the head and neck may reduce migraine headache symptoms. Trigger-point injections also may reduce people’s dependence on drugs, which sometimes can trigger additional headaches.
Aspirin, ibuprofen, and naproxen may play a preventative role. The drug—or combination of drugs that works best—depends on the individual. Unfortunately, overuse of these medications is a risk factor for chronic daily headaches.
Erenumab is a new FDA-approved treatment for migraines. It is part of a class of medications called calcitonin gene-related peptide (CGRP) monoclonal antibodies, which significantly reduce the frequency of migraine headaches.
Occipital-Nerve Stimulation. Occipital-nerve stimulation can control intractable migraines. Randomized trials showed significant improvement of daily pain scores, as well as significant decreases in the number of headache days in those who received occipital-nerve stimulation. In 2014, the FDA approved a battery-powered device called the Cefaly headband to prevent or reduce the number of migraine episodes by limiting pain signals.
Exposure to Narrow-Band Green Light. Approximately 80 percent of migraine sufferers report light sensitivity. Harvard researchers found that exposing migraine sufferers to narrow-band green light significantly reduced this side-effect and decreased pain.
Interstitial Cystitis
Interstitial cystitis (IC) is a complex condition characterized by an inflamed bladder wall, a scarred or stiffened bladder, diminished bladder capacity, and bleeding within the bladder. The exact cause of IC is unknown, but some believe there could be a defect in the lining of the bladder. IC is more common in women. When it occurs in men, the symptoms often overlap with prostate problems. Most people with IC are diagnosed in their 40s, but it can happen at any age.
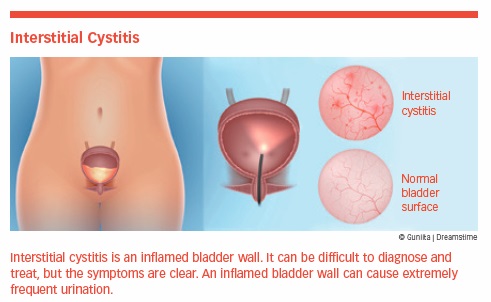
The most commonly reported symptom is frequent urination—up to 60 times a day in some cases. Other symptoms include: chronic pelvic pain, pressure, or tenderness, and pain during intercourse. Combined, these can have a profound negative effect on quality of life.
Many people with IC report that certain types of food trigger symptoms, including citrus foods, chocolate, caffeine, spicy foods, foods rich in potassium, and carbonated beverages. Stress can’t cause IC, but it can make it worse. A diagnosis may require a variety of procedures and medical opinions.
Treatment often includes nonsteroidal anti-inflammatories, antidepressants, antihistamines, and pentosan polysulfate sodium (Elmiron), which is FDA-approved for the treatment of IC.
Other therapies include distention of the bladder, medications placed directly into the bladder, surgery, and transcutaneous electrical nerve stimulation (TENS). Guided imagery and acupuncture have been effective in some cases.
Irritable Bowel Syndrome
Irritable bowel syndrome usually starts in early adulthood, and it affects more women than men. IBS doesn’t permanently damage the intestines, nor does it lead to serious diseases, such as cancer. The cause of IBS is unknown—it can’t be traced to any single condition, but research suggests that people with IBS have a sensitive colon, which overreacts in response to triggers, including certain foods and stress, that wouldn’t bother most others.
IBS is often diagnosed when other gastrointestinal conditions have been ruled out. No specific test can confirm its presence.
The most common symptoms are pain (often below the navel), stomach cramps, bloating, constipation, and/or diarrhea. These can worsen after eating large meals or fatty foods; taking certain medicines; eating wheat, rye, barley, or chocolate; and drinking milk, alcohol, or beverages containing caffeine, like coffee, tea, or soft drinks.
Most people control their symptoms with diet, stress-management techniques, and medications, including the antibiotic rifaximin. Prescription medications can decrease diarrhea, control colon muscle spasms, and reduce pain.
A study at the Mayo Clinic found that those with IBS may benefit from taking pregabalin (Lyrica), a drug commonly used to treat fibromyalgia. To address the psychological components of IBS, relaxation training, meditation, yoga, exercise, avoiding stressful situations, and getting quality sleep can help.
Myofascial Pain Syndrome
Myofascial pain syndrome (MPS) is characterized by trigger points, which are tight, sensitive muscle spasms that occur most often in the neck and back. These spasms restrict range of motion, come and go without warning, usually affect one side of the body, and may cause pain that radiates to adjacent areas.
The cause is unknown, but MPS is common among those who engage in repetitive-motion activities. Staying in one position for too long, overusing muscles, having a prior injury, poor sleep patterns, and stress also might cause MPS.
Pain medication, antidepressants, massage, and relaxation techniques can be effective. Direct, sustained (and perhaps painful) pressure on the sensitive part of the muscle can reduce tightness and pain. A few minutes of pressure can provide relief for hours or days. In cases where the pain is severe and limits normal activities, a physician may consider trigger-point saline injections. Botulinum toxin A (Botox) appears to be a promising therapy.
Osteoporosis
Osteoporosis is a progressive disease that causes bones to become thin and fragile. It’s estimated that 50 percent of women over the age of 50 are at risk of having a fracture caused by osteoporosis. Older men who’ve sustained a minor fracture are as likely to have a subsequent fracture as women.
Osteoporosis is the cause of 1.5 million fragility bone fractures (those related to a fall from a standing height or less) a year. Half of these fractures occur in the spine. The consequences of untreated osteoporosis and vertebral compression fractures can be serious, including lung disease.
Fewer than 30 percent of postmenopausal women and 10 percent of men with a prior fragility fracture are treated for osteoporosis. The Journal of General Internal Medicine reported that too few women at risk for osteoporosis were being tested, while too many without a risk factor were being screened for the disease with a bone-density scan.
Many risk factors are controllable:
- Low estrogen (women)
- Low testosterone (men)
- Low levels of calcium and/or vitamin D
- Anorexia
- Anti-seizure drug use
- Inactive lifestyle
- Cigarette smoking
- Excessive alcohol use
- Use of oral steroids
A study presented at the Endocrine Society’s Annual Meeting in March 2018 found that the heart-healthy Mediterranean diet pattern appeared to benefit bones and muscles in a sample of healthy older women.
Gender, age, race, and fragility fractures are also risk factors, but they can’t be controlled. Monitoring these factors may allow you to lower the risk or take preemptive steps before osteoporosis fully develops.
Beware of Fractures
A hip fracture almost always requires hospitalization and major surgery. It can impair a person’s ability to walk unassisted and may cause prolonged or permanent disability, or even death.
Spinal fractures result in height loss, severe back pain, and deformity. Although some people with osteoporosis experience no pain, others have intense pain caused by fractures and muscle spasms.
The long-term effects of untreated osteoporosis are detrimental and include impaired lung capacity, depression, low self-esteem, and increased risk of fractures.
Treatment. Pain associated with osteoporosis is treated by a variety of traditional and alternative therapies, including heat, ice, transcutaneous electrical nerve stimulation (TENS), exercise, massage, and relaxation. Vertebral augmentation, including Kiva implants, kyphoplasty and vertebroplasty, are examples of surgical procedures described in Chapter 3.
Among the drugs approved for osteoporosis are the bisphosphonates alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and zoledronic acid (Reclast). The FDA-approved twice-yearly injectable drug denosmab (Prolia) for the treatment of postmenopausal osteoporosis.
Researchers continue to discover new methods that could potentially lower the risk of osteoporosis. For example, older men and women who have one or two glasses of beer or wine a day appear to have stronger bones than both non-drinkers and heavy drinkers. However, it’s important to consider the potential benefits versus the risks, and most health-care professionals advise that if you don’t drink alcohol, this is not a reason to start.
Pelvic Floor Dysfunction
Pelvic floor dysfunction historically has been associated with women but can occur in men as well. The common denominators are pain in the front part of the pelvic region that can be dull, sharp, steady, or intermittent.
Long-term infection and endometriosis are two causes of PFD in women. Chronic pelvic pain may be caused by irritable bowel syndrome, interstitial cystitis, or muscle spasms. These may be compounded by psychological factors, such as depression or stress. Childbirth, trauma to the pelvic region, obesity, nerve damage, and some surgeries can also cause PFD.
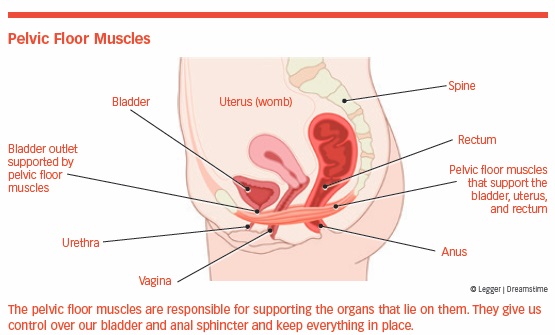
In men, symptoms are often related to the intestines or urinary tract and mimic those of prostatitis, such as urinary frequency, urgency, difficulty in starting urination, erratic flow, and pelvic-floor pain.
Both men and women struggle to get an accurate and timely diagnosis of this condition. Diagnosis often involves a process of elimination that might take months or years, and should include a thorough medical history, physical exam, and laboratory tests, as well as imaging when needed.
Treatment
The most effective treatment for pelvic floor dysfunction is pelvic floor rehabilitation. Symptoms such as bladder and bowel problems, as well as pelvic pain, may be relieved by as much as 80 percent with this method.
This involves physical therapy, biofeedback, pelvic floor muscle re-education, relaxation and strengthening exercises, and bladder/bowel training. PFD is a perfect example of how the coordination of care between a physical therapist and a pain physician provides optimal outcomes.
Treatment may include antibiotics (if infection has been detected), prescription and over-the-counter pain medications, relaxation exercises, physical therapy, nerve blocks, and surgery. In cases where no specific cause can be found, the goal of treatment may be to manage pain.
Pelvic pain in general is complex and may require an interdisciplinary team evaluation. The psychological status of the person is critical in making the diagnosis and determining proper treatment.
Shingles
One in three Americans will develop shingles during their lifetime. Most will get it once, but it’s possible to develop it a second or third time.
A viral disease, shingles causes a rash or blisters on the skin. It’s the same virus—the varicella-zoster virus—that causes chickenpox. After chickenpox heals, the virus becomes dormant in the body, but can reemerge if a person’s natural resistance is compromised.
Your risk of shingles increases with:
- A weakened immune system
- Being over the age of 50
- Being ill
- Experiencing trauma
- Being under stress
Symptoms include itching, stabbing, or shooting pains. The skin appears red in the affected area. A tell-tale rash appears after a few days around the waistline or on one side of the face or trunk. Other symptoms include, fever, chills, headache, and an upset stomach.
There’s no cure for shingles, but treatment with antiviral medications—such as acyclovir (Zovirax), valacyclovir (Valtrex), and famciclovir (Famvir)—can help ease the pain and discomfort and reduce the duration of symptoms.
The shingles vaccines Zostavax, which was approved in 2006, has largely been replaced by Shingrix, which was approved in 2017 and is preferred by most physicians. The CDC recommends that healthy adults 50 years and older get two doses of Shingrix, two to six months apart.
Postherpetic Neuralgia
Postherpetic neuralgia (PHN) is a painful complication of shingles. Even after the blisters of shingles heal, nerve pain can remain. Although the pain gradually fades, it can persist for years.
Not everyone with shingles develops post-herpetic neuralgia, but the older you are when you first get shingles, the more likely you are to develop PHN. Half of those over 60 who get shingles develop PHN, while 75 percent of those over 70 get the condition.
The primary symptom of PHN is severe unilateral pain that can lead to insomnia, weight loss, and depression. Other symptoms include:
- Sharp, jabbing, burning, deep, or aching pain
- Itching or numbness
- Unusual sensitivity to touch and temperature change
- Weakness (rarely)
The shingles vaccine can help prevent the disease (and thus its complications) in adults over 60, and it can relieve the pain of post-herpetic neuralgia if the disease occurs.
Skin patches containing lidocaine or capsaicin, antidepressants, anti-seizure medications, painkillers, opioids, and transcutaneous electrical nerve stimulation (TENS) can be effective for many in relieving the pain. Aggressive treatment of acute-phase shingles with sympathetic nerve blocks may decrease the chances of developing PHN.
Treatment with intravenous and oral antiviral medications, such as acyclovir (Zovirax), may reduce nerve pain. Newer anti-neuropathic pain agents, such as pregabalin (Lyrica), also may be effective in treating PHN.
Surgery
Although surgery is often a necessity it can lead to chronic pain. In certain operations—limb amputation, lung surgery, breast surgery, gallbladder surgery, hernia surgery—the incidence of postoperative chronic pain ranges from 11 to 47 percent, noted a study published in the journal Anesthesiology. According to Practical Pain Management 10 percent of surgery people may experience chronic pain at least three to six months following surgery.
Risk factors associated with postoperative chronic pain can be classified as factors existing before surgery (pre-existing pain intensity, obesity, or genetic predisposition), factors that develop during surgery (nerve damage or the effects of anesthesia), and those associated with treatment after surgery (radiation, chemotherapy).
Treating postoperative chronic pain is as complex as relieving chronic pain caused by any other condition. It often requires a team approach and includes pain medications, physical therapy, and counseling.
TMJD
Temporomandibular joint disorders (TMJD) refer to a group of symptoms affecting the joints connecting the lower jaw to the skull. Symptoms include difficulty opening the mouth, pain (jaw, face, ear), headaches, and toothaches, as well as painful clicking, popping, or grating in the jaw when opening or closing the mouth.
Clenching and grinding your teeth, poor head and shoulder posture, an inability to relax, and lack of sleep can cause TMJD. Arthritis, fractures, joint degeneration, or structural abnormalities also can cause contracted muscles and pinched nerves in the jaw, head, and neck.
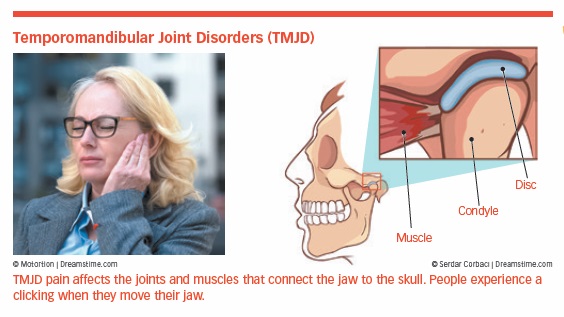
Suggested treatments include, mouth guards, massage, moist heat, cold applications, and exercises to help relax the jaw. More aggressive therapy involves muscle relaxants, NSAIDs, orthodontics, and, very rarely, reconstructive surgery. TMJD can go away temporarily and return later. Note: Some health insurance contracts have limited coverage for TMJD.
People with chronic jaw pain appear to be more sensitive to pain in other parts of the body. Several genes may be linked to TMJD, which may lead to new drug treatments. A connection between TMJD and depression and anxiety may exist.
Trigeminal Neuralgia
Trigeminal neuralgia occurs when a blood vessel puts pressure on the trigeminal or 5th cranial nerve, the largest of the 12 cranial nerves.
Trigeminal neuralgia is considered one of the most painful conditions you can experience. It can be triggered by something as simple as brushing your teeth, causing sudden sporadic burning or shock-like facial pain along the path of the trigeminal nerve. The pain can last from a few seconds to a few minutes and may repeat itself. A less typical form causes a constant stabbing pain.
The pain can be incapacitating since the nerve travels along the side of your face, down through your jaw line. It also reaches the eye area and cheeks. Because of the location of the pain, trigeminal neuralgia is sometimes mistaken for a tooth problem, prompting unnecessary root canals in an attempt to alleviate the pain.
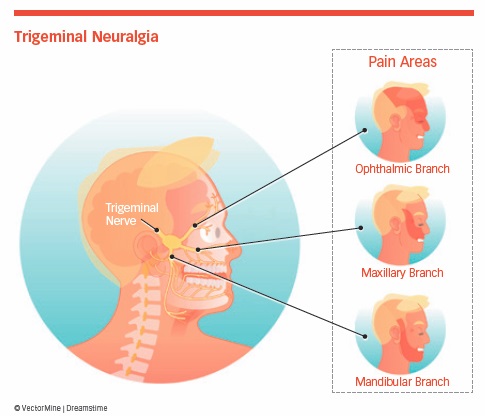
The distinguishing characteristic is a sudden, electric shock-like pain on one side of the jaw or cheek lasting for up to a couple of minutes. Attacks may occur one after the other, and can be triggered by talking, brushing the teeth, touching the face, chewing, swallowing, or even by a breeze touching the face.
Some trigeminal neuralgia episodes can last for months before disappearing for years.
The disorder is more common in women and mostly affects those over 50. Trigeminal neuralgia should be distinguished from a host of other causes of facial pain. A full history and physical examination, as well as imaging studies, may be required to make a diagnosis.
Treatment
Anti-seizure medications are often used in treatment. The drugs carbamazepine (Tegretol, Carbatrol) and oxcarbazepine (Trileptal) are considered first-line therapy. Researchers at the University of Zurich have shown that a substance temporarily called BIIB074 appears to inhibit the pain of trigeminal neuralgia.
Nerve blocks or radiofrequency ablation of the trigeminal ganglion should be considered before surgery. If medication or radiofrequency ablation fails to relieve pain, surgery may be recommended.
Gamma knife radiosurgery (GKRS) is a treatment option. GKRS is a non-invasive, outpatient treatment that aims narrow beams of radioactive cobalt at the trigeminal nerve. Ninety percent of people have significant pain relief within an average of four weeks after GKRS, and 80 percent have a significant improvement in quality of life.
The post 2. The Origins of Pain appeared first on University Health News.