8. Prevention: Managing Risk Factors
Heart failure is largely preventable because it is often the result of other diseases. Preventing or managing those underlying diseases lowers the risk of heart failure. Taking aggressive control of high blood pressure, losing weight, controlling diabetes, avoiding alcohol abuse and illicit drugs, and taking measures to prevent coronary artery disease all improve your chances of avoiding heart failure.
It is particularly important in men and African Americans, who are more likely to develop heart failure than women and Caucasians. According to the Health, Aging, and Body Composition Study, a large proportion of heart failure deaths and hospitalizations in this population are attributed to modifiable risk factors.
Mortality Rate Dropping
The number of individuals who die from coronary artery disease is dropping. This decline is attributed largely to the use of evidence-based medical therapy for prevention of a second heart attack and to changes in lifestyle.
Lowering high levels of triglycerides (fats that circulate in the blood) and low-density lipoprotein (LDL) plays a major role in preventing coronary artery disease. However, low LDL and total cholesterol may be a marker of poor outcomes in heart failure patients. Studies of patients with cardiac cachexia (body-wide loss of muscle mass due to heart failure) and end-stage heart failure have shown that the likelihood of dying rises as total cholesterol levels fall. This challenges the theory that everyone with high cholesterol should take statins to lower cholesterol.
Despite this so-called “cholesterol paradox,” heart failure patients who take statins may reduce their risk of heart attack and death by 20 to 25 percent. In another paradox, heart failure patients who are heavier and have slightly higher blood pressure actually do better than their thinner peers whose blood pressure is normal.
Early identification of patients with heart muscle dysfunction, which occurs before heart failure develops, allows for appropriate medical treatment that may prevent the progression of heart failure.
Stop It from Getting Worse
Once heart failure has started, heart function may never return to normal. The goal becomes preventing heart function from deteriorating further. Patients must take medications, even when their symptoms are absent or improve. The use of angiotensin-converting enzyme inhibitors and beta-blockers or appropriate interventions—for example, replacing aortic valves narrowed by calcium deposits or performing coronary bypass surgery—can improve heart muscle function in certain patients.
Remote-monitoring techniques using internal and external devices appear to help prevent further deterioration by enabling physicians to intervene early to prevent hospitalization. One remote monitoring device reduced hospital admissions for heart failure by 43 percent and readmissions by 78 percent.
For the best care and latest techniques to maintain the heart’s pumping power, getting treatment at a medical center with special expertise in heart failure is highly recommended. Advanced multidisciplinary care can reduce hospitalizations and improve quality of life.
Prevent It or Manage It
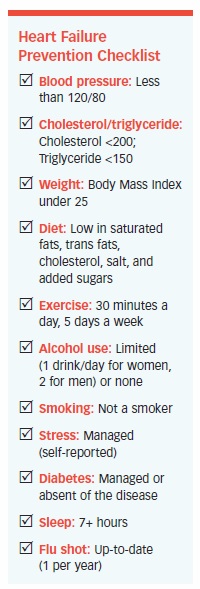
The “Heart Failure Prevention Checklist” contains 11 ways you can either prevent or manage heart failure. How many apply to you?
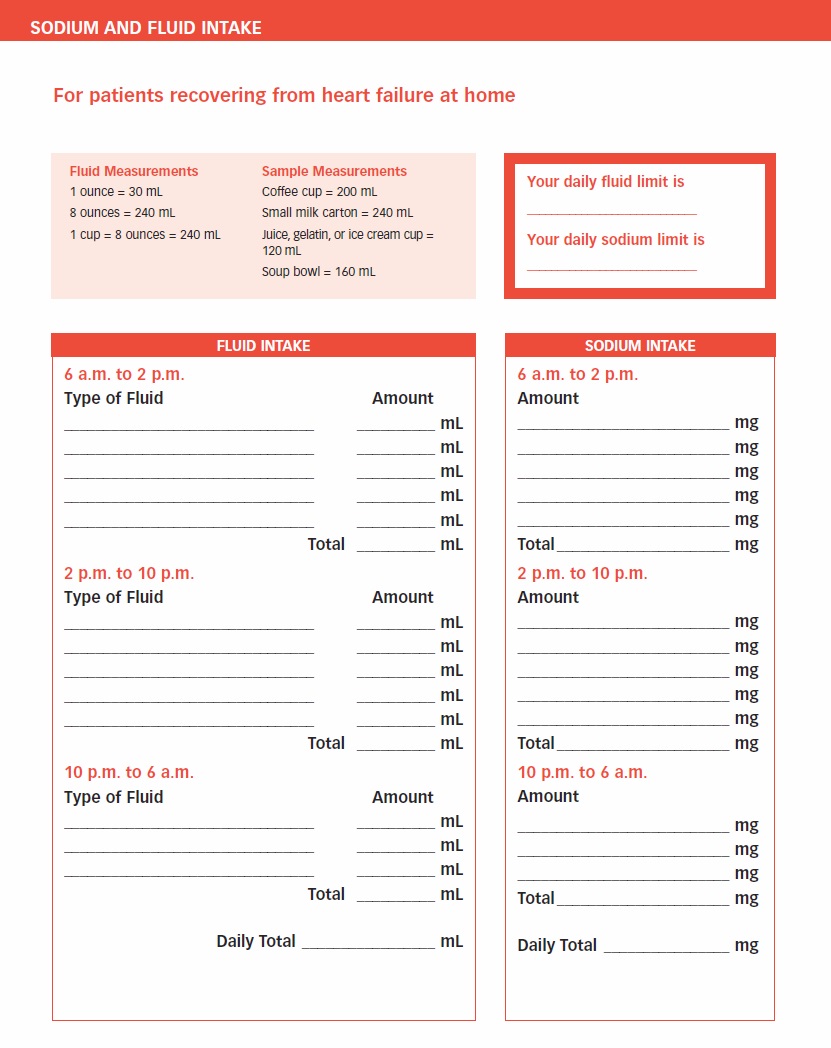
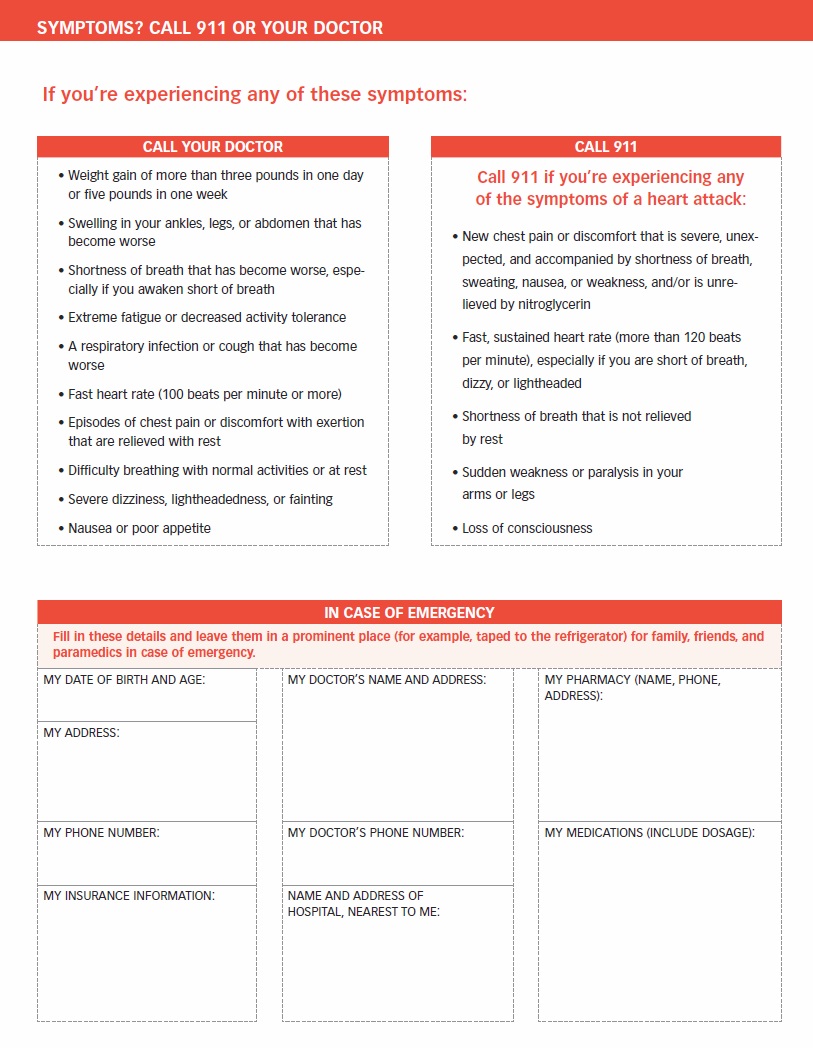
Taking an active role in disease management can be challenging, but it is essential for living the best life possible. We hope the content in this report has given you practical, hopeful and actionable information. The forms and resources on the following pages can further guide your efforts in living well.
The post 8. Prevention: Managing Risk Factors appeared first on University Health News.
Read Original Article: 8. Prevention: Managing Risk Factors »


