Early Glaucoma Detection Is the Key to Sight-Saving Treatment
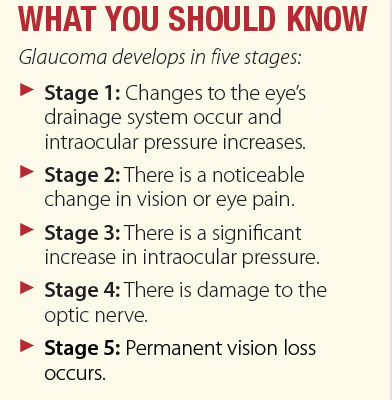
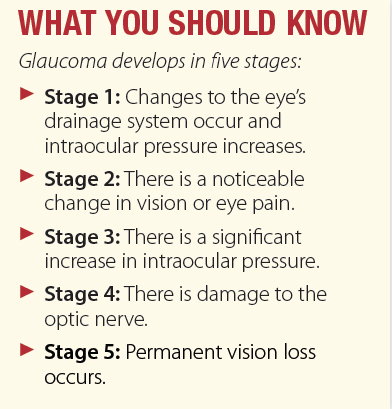
Glaucoma is often referred to as the “silent thief of sight” because it progresses slowly and painlessly, often without noticeable symptoms. It causes damage to the optic nerve, which is responsible for transmitting visual information from the eye to the brain. As glaucoma progresses, this damage leads to vision loss that can result in blindness if left untreated. By detecting glaucoma early, before significant optic nerve damage occurs, treatment can be initiated to preserve remaining vision and prevent further vision loss.
Risk Factors
Primary open-angle glaucoma (POAG), which is the most prevalent type of glaucoma, occurs as often in women as men; however, women are more likely to develop angle-closure glaucoma and normal tension glaucoma—two less common forms of this condition. Other factors that increase glaucoma susceptibility include family history—especially if a close relative has been diagnosed—and ethnicity. Blacks are more prone to glaucoma, often developing it earlier and experiencing more severe forms, while Hispanics, Latinos, and people of East Asian descent also have increased susceptibility.
Elevated intraocular pressure (IOP) is a significant glaucoma risk factor, though normal pressure doesn’t guarantee immunity. Medical conditions like diabetes, hypertension, and eye trauma can further compound risk, as can thinner corneas, prolonged steroid use, nearsightedness, and lifestyle factors such as smoking and sedentary habits. “Glaucoma damage is permanent and irreversible; therefore early detection is paramount. It’s important for patients over 40 years of age and especially those with risk factors, such as a positive family history, to have a complete eye examination, including measurement of IOP, inspection of the eye’s drainage angle,
examination of the optic nerve, measurement of the thickness of the cornea, and testing of peripheral (side) vision,” says Ana Alzaga Fernandez, MD, assistant professor of ophthalmology at Weill Cornell Medicine.
Eye Drops and Other Medications
While there is no cure for glaucoma, a variety of treatment options are available to manage it.
From prescription eye drops and oral medications to laser therapy and surgery, the choice of treatment depends on the type and severity of glaucoma, the patient’s overall health, and their ability to adhere to treatment regimens. “The treatment of glaucoma is geared mainly toward modifying IOP. The ophthalmologist will tailor the appropriate IOP range for each patient according to their risk factors and testing results,” says Dr. Alzaga Fernandez.
Prescription eye drops are often the first line of treatment. They work by either reducing the production of aqueous humor (the fluid inside the eye) or improving its drainage. In some cases, oral medications may be prescribed alongside or instead of eye drops to help lower IOP. Oral medications are usually reserved for people who have difficulty tolerating or administering eye drops.
Laser and Surgical Treatments
Laser therapy is often used when eye drops or oral medications are insufficient or not well-tolerated. Types of laser therapy for glaucoma include selective laser trabeculoplasty, which targets and improves drainage to reduce IOP; laser peripheral iridotomy, which is typically used for angle-closure glaucoma, and laser cyclophotocoagulation, which reduces the production of aqueous humor by treating the part of the eye that produces the fluid. “Once the treatment has begun, IOP is monitored regularly along with other things such as peripheral vision. If IOP is maintained within the ideal range, progression of the condition is more likely to be limited,” says Dr. Alzaga Fernandez.
When medications and laser therapy are ineffective or inadequate in controlling disease progression, surgery may be recommended. Common surgical procedures for glaucoma include trabeculectomy, minimally invasive glaucoma surgery, and implantation of glaucoma drainage devices. The aim of each of these procedures is to help drain excess fluid out of the eye to reduce IOP.
Treatment Adherence
Keeping follow-up appointments and adhering to prescribed medications are critical for patients with glaucoma. “Given the condition’s asymptomatic nature, it’s vital to schedule routine visits every three to four months for most glaucoma patients, and every six months for glaucoma suspects. This ensures that they can be closely monitored for any signs of disease progression and have timely treatment adjustments, if necessary,” says Dr. Alzaga Fernandez.
Early glaucoma diagnosis can help prevent vision loss. The first step is scheduling a vision exam. It’s important for women with glaucoma and those at risk for the disease to work closely with their eye doctor so IOP can be monitored and, if necessary, treated.
The post Early Glaucoma Detection Is the Key to Sight-Saving Treatment appeared first on University Health News.
Read Original Article: Early Glaucoma Detection Is the Key to Sight-Saving Treatment »