6. Drug Treatments for Cholesterol
Despite all their best efforts, some people still can’t keep their lipids and cardiovascular risk at acceptable levels. If you’re one of them, you’ll need a medication to help control your cholesterol and reduce your risk of heart attack and stroke.
Statins remain the cornerstone of cholesterol-lowering drug therapy, but a number of other prescription medications, and a few nonprescription options, also can help you improve your lipid profile. Trouble is, research suggests that many people whose lipid levels aren’t where they should be aren’t undergoing optimal medical treatment or doing all they can to reduce their cholesterol.
For instance, troubling data from a study published in 2018 in Circulation indicated that only about half of people with familial hypercholesterolemia and others with severely high LDL cholesterol levels were being treated with statins, and even fewer were on high-intensity statin therapy. Other evidence has found gender differences in guideline-recommended statin therapy, suggesting that women are less likely than men to receive high-intensity statins.
So, to optimize your cholesterol and cardiovascular risk management, it’s vital to talk to your doctor about whether or not you need cholesterol-lowering treatment. If so, discuss all your treatment options with your doctor. In this chapter, we look at the medications and over-the-counter products commonly used to improve cholesterol levels.
Statins
They’re known scientifically as 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors. Most people know them as statins.
Statins are among the most widely prescribed medications in the world—they’re so universally used that some people have joked that they should be added to the water supply. Statins can effectively lower LDL and total cholesterol, and they have some triglyceride-lowering and anti-inflammatory effects. They also may modestly raise levels of beneficial HDL cholesterol. Yet, statins have important side effects that you need to know about.
How Statins Work
Statins block the action of an enzyme (HMG-CoA) responsible for cholesterol production in the liver. Most of the drugs are available in generic forms.
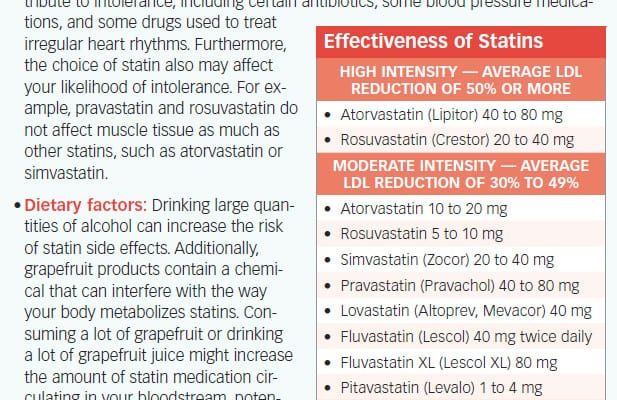
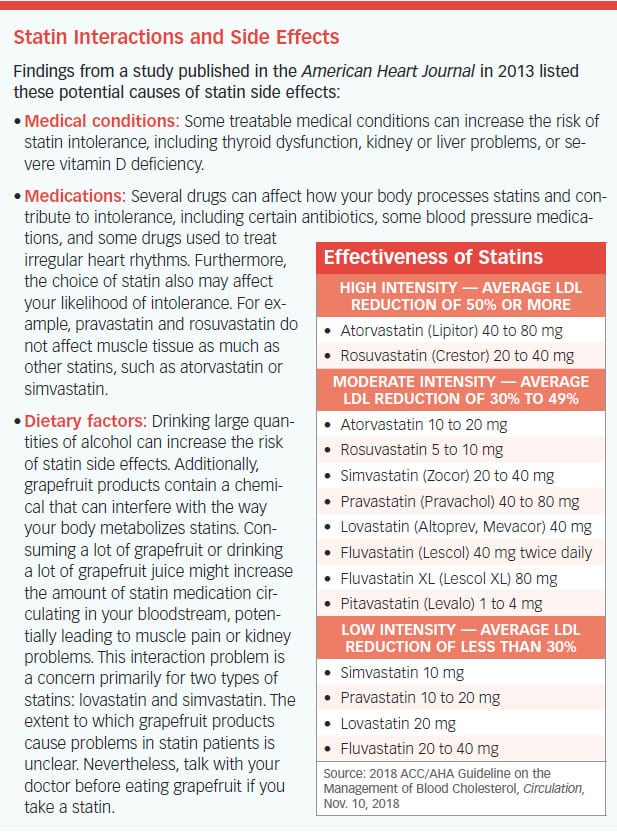
Although they belong to the same drug class, not all statins are equal in terms of their potency and the degree to which they reduce LDL—atorvastatin and rosuvastatin are among the most potent statins, while fluvastatin and pravastatin are among the least potent (see “Statin Interactions and Side Effects”).
Also, while most studies have found that statins can benefit people irrespective of age, some research has raised questions about how well the drugs work in relatively healthy older individuals. A study published in 2018 in BMJ that included 46,864 older adults followed a median of 5.6 years found that statin treatment offered no benefit in terms of primary prevention of atherosclerotic cardiovascular disease or death from all causes after age 74, except in people with diabetes. In those with diabetes, the benefits of statins waned after age 85 and disappeared in those in their 90s.
Helping More Than Just LDL
Statins may have many pleiotropic beneficial effects that are independent of the drugs’ intended action of LDL reduction.
Stabilizing Plaque. Some research suggests that high-intensity statin therapy may help stabilize coronary atherosclerotic plaques and make them less susceptible to rupture and cause heart attacks and strokes. In the 2018 PARADIGM trial, 1,255 people with no documented coronary artery disease underwent serial coronary computed tomographic angiography scans at an interval of two or more years. Researchers identified 1,079 coronary artery plaque lesions in 474 people not taking statins and 2,496 such lesions in 781 statin users. Statin users had a slower progression of overall coronary atherosclerosis volume, lower annual incidence of high-risk plaques, and increased plaque calcification (believed by some researchers to help reduce the risk of plaque ruptures).
Other evidence suggests that statins also can slow—and potentially reverse—the progression of atherosclerotic plaque. The Study of Coronary Atheroma by Intravascular Ultrasound: Effect of Rosuvastatin Versus Atorvastatin (SATURN) compared the effects of 80 milligrams (mg) of atorvastatin versus 40 mg of rosuvastatin (the highest doses available) on plaque progression in 1,039 people with stable coronary artery disease. About 63 percent of people taking atorvastatin and 68 percent of those on rosuvastatin experienced a regression, or reversal, of their atherosclerosis.
Anti-Inflammatory. Statins have anti-inflammatory effects. Some studies have shown that even if you have a normal LDL level, you still may be at increased risk of cardiovascular events if you have elevated levels of inflammatory markers such as C-reactive protein (CRP). In one trial—Justification for the Use of Statins in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER)—investigators reported that rosuvastatin reduced the risk of heart attack, stroke, and death by 44 percent in more than 17,000 people with normal LDL but elevated CRP levels.
Blood Pressure. Statins aren’t thought of as antihypertensive medications, but recent research suggests that for many patients with high blood pressure, adding statins to their antihypertensive medication regimen may make a huge difference. In the Heart Outcomes Prevention Evaluation-3 (HOPE-3) trials, researchers reported that a combination of statin therapy and antihypertensive therapy significantly lowered the risk of cardiovascular events among intermediate-risk patients with high blood pressure. However, the researchers found that the outcomes with the combination of rosuvastatin and antihypertensive therapy (candesartan plus hydrochlorothiazide) were not significantly better compared with those of rosuvastatin alone, emphasizing the importance of the statin drug.
Tolerating Statins
While most patients have no problem taking statins, the drugs do have side effects just like any other medication. The side effects are more severe as the statin dose and potency increase. The most common statin side effects include headache and gastrointestinal symptoms, but other potential side effects include:
- Myopathy. An estimated 5 to 20 percent of statin users report muscle pain and stiffness, or myopathy. Rarely, statin users may experience rhabdomyolysis, a potentially life-threatening muscle breakdown. Some statin users have taken coenzyme Q10 (CoQ10) supplements to counter their myopathy. In a 2018 meta-analysis of 12 randomized trials involving 575 statin patients, researchers concluded that use of CoQ10 effectively eased statin-related muscle symptoms, reported the Journal of the American Heart Association.
- Liver abnormalities. Statins can cause elevations in liver enzymes, suggesting potential liver damage. So, your doctor may recommend liver-function tests in certain situations, such as when you start statin therapy, change the dose or the type of statin, or if you begin taking other medications metabolized by the same pathway in the liver as statins.
- Blood-sugar elevations. Studies have found an increase in blood sugar among statin users. These findings prompted the FDA to add to the statin safety information an advisory that the medications may slightly raise blood sugar, enough to push some patients’ glucose levels across the threshold of diabetes. Although two earlier meta-analyses found only a 9 to 13 percent increased risk of diabetes associated with statin use, a more recent study (involving 9,535 people over age 45) found that statin use was associated with a 38 percent higher risk of type 2 diabetes, particularly in those who were overweight/obese or had prediabetes (British Journal of Clinical Pharmacology, online March 5, 2019). Interestingly, another study found that statin therapy was associated with a reduced risk of diabetic eye disease (retinopathy) and need for treatments for vision-threatening retinopathy in Taiwanese adults with type 2 diabetes and dyslipidemia (JAMA Ophthalmology, online Jan. 10, 2019).
- Cognitive problems. Although some research suggests that statins may slow the progression of dementia and improve memory, as a rare side effect, some patients may experience cognitive problems, such as forgetfulness and mental “fogginess,” while taking a statin. Consequently, the FDA has added to the statin safety information a notice about possible cognitive problems associated with statin use. These side effects typically subside after stopping the medication. Overall, whether statins cause cognitive problems is unclear.
- Cataracts. In a study involving nearly 7,000 patients, statin users were 9 percent more likely than non-users to develop cataracts. Another study found an association between statin use and a greater likelihood of cataracts requiring surgery. But, although these studies have identified an association between statins and cataracts, a causal relationship has not been established.
Finding the Right Regimen
Some patients simply cannot tolerate statins; however, there are other cholesterol-lowering strategies, so you can find the one that works for you.
In one study, more than 72 percent of patients who were previously statin-intolerant were able to resume statin therapy, often with the help of dosing adjustments or switching to a different medication in the statin class. While most of the patients could return to a daily statin regimen, others could tolerate only intermittent therapy, taking the drugs every other day or as infrequently as once a week. The patients who resumed daily statin therapy overall achieved greater LDL reductions than those on intermittent therapy, but both groups experienced greater LDL reductions and were more likely to achieve their LDL goals compared with those who discontinued statin use, the study found.
The findings suggest that complete statin intolerance (an inability to take any statins) is relatively rare and that patients and their physicians just need to persevere in finding the right treatment regimen and rule out potential causes of statin side effects.
Stick with Your Statin Therapy
Given the extensive literature supporting the effectiveness of statins in preventing 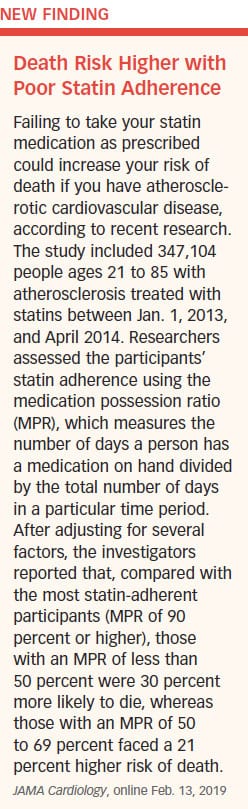 cardiovascular events, most experts agree that the benefits of statin therapy outweigh the risks associated with the drugs.
cardiovascular events, most experts agree that the benefits of statin therapy outweigh the risks associated with the drugs.
So, follow your physician’s recommendations for follow-up testing, and promptly report any statin-related side effects to your doctor. Take your statin exactly as prescribed, and do not stop taking your medication or otherwise alter your statin regimen without first consulting with your physician (see “Death Risk Higher with Poor Statin Adherence”).
Be patient. It may take time and several tries to find a cholesterol-lowering regimen that you can tolerate. If you absolutely cannot tolerate statins, or if you can tolerate only intermittent statin dosing, other cholesterol-lowering medications may be necessary to reduce your LDL level. Explore all your options to optimize your LDL and reduce your cardiovascular risk.
PCSK9 Inhibitors
If you’re among the people who cannot tolerate statins, a newer class of drugs—proprotein convertase subtilisin kexin type 9 (PCSK9) inhibitors—can reduce LDL to levels beyond what most statins can achieve. The first PCSK9 inhibitors—alirocumab (Praluent) and evolocumab (Repatha)—gained FDA approval in 2015.
The PCSK9s are given by injection every two weeks or once a month, compared with daily oral statin therapy. The drugs are indicated as a complement to a heart-healthy diet and maximally tolerated statin therapy for adults with heterozygous familial hypercholesterolemia or those with coronary heart disease who require additional reductions in LDL.
 The latest cholesterol guidelines from the ACC and AHA recommend that PCSK9 inhibitors be considered for patients with atherosclerotic cardiovascular disease at very high risk whose LDL cholesterol remains at 70 milligrams per deciliter (mg/dL) or higher on maximally tolerated statin therapy and ezetimibe (Zetia—read more about this drug later in this chapter), as well as those with familial hypercholesterolemia whose LDL remains above 100 mg/dL despite the statin/ezetimibe combination.
The latest cholesterol guidelines from the ACC and AHA recommend that PCSK9 inhibitors be considered for patients with atherosclerotic cardiovascular disease at very high risk whose LDL cholesterol remains at 70 milligrams per deciliter (mg/dL) or higher on maximally tolerated statin therapy and ezetimibe (Zetia—read more about this drug later in this chapter), as well as those with familial hypercholesterolemia whose LDL remains above 100 mg/dL despite the statin/ezetimibe combination.
How They Work
Whereas statins decrease the amount of cholesterol the liver synthesizes (reducing LDL) from the blood, the PCSK9 inhibitors are antibodies that block the action of a protein (PCSK9) that degrades the receptors on the liver’s surface that remove LDL. The result is a greater number of receptors left to pull the particles carrying LDL from the blood. With this mechanism of action, the PCSK9s produce significant reductions in LDL in addition to statin therapy—an average of 36 to 59 percent for alirocumab and an average of 60 percent for evolocumab.
Reductions in Cardiovascular Risk
Not only do the PCSK9s reduce LDL, but a seminal international trial showed that they also can cut the risk of cardiovascular events, such as heart attack and stroke.
In the Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial, 27,564 patients with cardiovascular disease treated with moderate- to high-intensity statin therapy received evolocumab (every two weeks or once a month) or a placebo and were followed every 12 weeks for an average of 2.2 years. Compared with placebo, evolocumab lowered LDL from a median of 92 mg/dL to 30 mg/dL, a 59 percent reduction, the study found.
The drug reduced the risk of the study’s primary endpoint—a composite of heart attack, stroke, cardiovascular death, hospitalization for cardiac chest pain (angina), or revascularization—by 15 percent. More specifically, the drug reduced the composite of heart attack, stroke, and cardiovascular death by
25 percent.
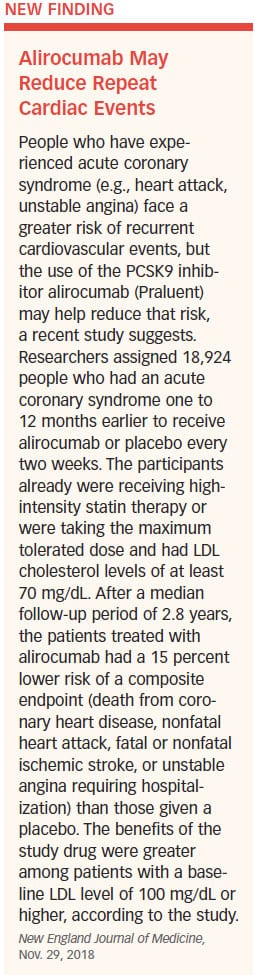
A more recent study suggests that patients with a history of acute coronary syndrome can derive similar benefits from the other PCSK9 inhibitor, alirocumab (see “Alirocumab May Reduce Repeat Cardiac Events”).
Lingering Questions
Despite the benefits of the PCSK9s, some uncertainties regarding the drugs remain. For instance, the long-term side effect profile of the new medications hasn’t been fully clarified or documented. However, the drugs, for the most part, appear to spare patients the muscle aches and stiffness associated with statin use.
The most common side effects associated with the PCSK9s include mild cold- or flu-like symptoms, as well as itching, swelling, or other reactions at the injection site. In the FOURIER trial, aside from a higher rate of injection-site reactions, no significant differences in adverse events (including new cases of diabetes or cognitive problems) occurred between the two study groups.
Just remember that, like statins, the PCSK9 inhibitors should be considered as an adjunct to, not a replacement for, a heart-healthy diet and regular exercise. At least for now, the drugs are intended to complement, not replace, statin therapy. If you can’t tolerate statins, discuss alternative statin regimens and other medications that can help you manage your cholesterol.
How Low Should You Go?
Newer drugs like the PCSK9 inhibitors, as well as other medications used to augment statin therapy, have spurred interest in reducing LDL cholesterol to levels lower than were thought possible before, such as the average 30 mg/dL level achieved in the FOURIER trial. In fact, a subsequent analysis of FOURIER found that as LDL levels dropped, so did the risk of cardiovascular outcomes.
Increasing evidence supports the value of aiming for these ultra-low LDL levels in the highest-risk patients, such as those with established cardiovascular disease or familial hypercholesterolemia, including those with already low LDL levels. In a 2018 meta-analysis of multiple studies published in JAMA Cardiology, researchers sought to determine if reducing LDL in patients with levels of 70 mg/dL or less, using statins and other cholesterol-lowering medications, would confer additional benefits. They found that the relative risk of major vascular events was reduced by 21 to 22 percent for each 38.7 mg/dL reduction in LDL achieved by using statins or non-statins, such as ezetimibe and evolocumab. The reductions in risk occurred in patients starting with a median LDL as low as 63 mg/dL and achieving levels as low as a median of 21 mg/dL, the investigators wrote. Importantly, the LDL reductions were not associated with an increased risk of adverse side effects.
Some experts also advocate more aggressive LDL lowering as primary prevention for patients without documented cardiovascular disease but with other factors, such as markedly elevated LDL, high blood pressure, type 2 diabetes, obesity, or a strong family history of heart disease. In these cases, statin therapy combined with other medications, like ezetimibe, may be used to reach target goals.
Overall, you and your health-care team can decide about the efficacy and safety of aiming for lower LDL targets and the combination of medications that can help you reach your goal.
More Drug Choices
Your physician may discuss other drug options with you, depending on your individual circumstances.
Ezetimibe
While statins reduce the amount of cholesterol your body produces, ezetimibe lowers the amount of cholesterol absorbed through your small intestine. A combination pill (brand Vytorin) combines ezetimibe with simvastatin and is widely prescribed.
Ezetimibe can lower LDL by an average of about 18 to 20 percent, compared with LDL reductions of up to 50 to 60 percent seen with high-potency statin therapy. The drug also may produce slight reductions in triglycerides and slight increases in HDL. Ezetimibe may cause some mild gastrointestinal side effects, but otherwise it is generally well tolerated.
The latest ACC/AHA cholesterol guidelines recommend adding ezetimibe to maximally tolerated statin therapy in patients with atherosclerotic cardiovascular disease at high risk whose LDL remains at 70 mg/dL or higher, and also for patients with familial hypercholesterolemia whose LDL remains above 100 mg/dL despite statin therapy. The guidelines note that “it may be reasonable” to add ezetimibe to maximally tolerated statin therapy for people with diabetes whose 10-year cardiovascular risk is 20 percent or greater, and also to add ezetimibe to moderate-intensity statin therapy for intermediate-risk patients who would benefit from more aggressive LDL lowering but who cannot tolerate high-intensity statins.
Overall, if you have heart disease and are already on statin therapy, you could safely gain extra benefits by adding ezetimibe to further lower your LDL. And, if you can’t tolerate a statin due to side effects or if a statin isn’t sufficiently lowering your LDL on its own, ask your doctor if ezetimibe may be reasonable to add for further reducing your LDL and, presumably, your cardiovascular risk.
Bile Acid Sequestrants
This older class of medications includes cholestyramine (Prevalite), colestipol (Colestid), and colesevelam (Welchol). These drugs prompt the liver to convert more cholesterol into bile acids, subsequently lowering LDL levels by 10 to 15 percent with low doses and up to 25 percent with higher doses. Given the modest LDL reductions that bile acid sequestrants can produce, they’re usually prescribed only as an adjunct to statins or in people with statin intolerance.
Side effects include constipation, gas, bloating, heartburn, diarrhea, and nausea.
Fibrates
These drugs, such as fenofibric acid (Antara, Tricor) and gemfibrozil (Lopid), reduce fat production in the liver and are generally used to treat patients with high triglycerides. Side effects include nausea and stomach pain.
Niacin
 Niacin (vitamin B3, nicotinic acid) is important for converting food into energy, just like all B vitamins. But in high doses, niacin can be used to treat dyslipidemia. Prescription-strength doses (Niacor, Niaspan) can mildly reduce LDL, lower triglycerides, and give your HDL a boost.
Niacin (vitamin B3, nicotinic acid) is important for converting food into energy, just like all B vitamins. But in high doses, niacin can be used to treat dyslipidemia. Prescription-strength doses (Niacor, Niaspan) can mildly reduce LDL, lower triglycerides, and give your HDL a boost.
However, research suggests that increasing HDL levels doesn’t necessarily translate into reduced cardiovascular risk. For example, in the AIM-HIGH trial, niacin therapy improved HDL and triglyceride levels but provided no additional clinical benefit among statin patients with established cardiovascular disease and LDL levels below 70 mg/dL.
Prescription-strength niacin causes facial and neck flushing in many users. To reduce flushing, take a non-enteric-coated aspirin 30 to 40 minutes before taking niacin, and avoid spicy foods or stimulants, such as caffeine. Niacin may increase blood-sugar levels and may cause stomach upset, dizziness, headache, and blurred vision.
Niacin also can increase uric acid levels and contribute to painful gout. At high doses, niacin may contribute to liver damage and stomach ulcers. Considering these side effects, it’s best not to self-medicate with over-the-counter niacin supplements, but rather to use niacin with care only under your doctor’s supervision.
On the Horizon: Bempedoic Acid
Researchers are studying another drug that might be added to statin therapy to boost its LDL-lowering capabilities. Bempedoic acid is known as an ATP citrate lyase inhibitor, which reduces cholesterol production in the liver by blocking the action of an enzyme (ATP citrate lyase) that’s on the same pathway as the enzyme targeted by statins. However, bempedoic acid does not affect cholesterol production in the muscles, leading researchers to believe it may be less likely to cause the muscle side effects associated with statin use.
In a 2019 trial published in the New England Journal of Medicine, 2,230 people with atherosclerotic cardiovascular disease, familial hypercholesterolemia, or both were assigned to receive bempedoic acid or placebo in addition to their maximally tolerated statin therapy. All the participants had an LDL level of at least 70 mg/dL. At 12 weeks, compared with placebo, bempedoic acid reduced LDL by an average of 19.2 mg/dL (a 16.5 percent decrease from baseline), with no increase in adverse side effects, the researchers reported.
Help from Supplements
The medicinal properties of Chinese red yeast rice have been documented for about 1,200 years. But in more recent years, this herbal supplement has been the subject of controversy, despite evidence that it can reduce cholesterol.
That’s because red yeast rice contains substances known as monacolins, including monacolin K, which is identical to the active ingredient in the statin drug lovastatin (Mevacor). The FDA has labeled red yeast rice products containing more than trace amounts of monacolin K as “unapproved new drugs,” meaning they can’t be sold as dietary supplements.
Like any drug or supplement that can produce a therapeutic effect, red yeast rice may cause the same types of side effects and drug interactions as statins. Also, the National Center for Complementary and Integrative Health notes that some red yeast rice products contain a substance known as citrinin, which can cause kidney damage.
Inform your doctor if you use red yeast rice, and report any side effects. Better yet, if you need to reduce your cholesterol, ask your physician about other, more proven cholesterol-lowering therapies, such as statins.
Get Fishy
Diets containing the omega-3s eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are heart-healthy, but like many people, you may not consume enough dietary sources of these potent omega-3s. So, you might consider getting omega-3s from fish oil supplements to lower your cardiovascular risk.
EPA and DHA are polyunsaturated fats found prominently in fatty fish such as wild salmon, mackerel, tuna, and herring. Studies have found that diets rich in EPA and DHA can benefit heart health in several ways, such as lowering triglycerides, slightly reducing blood pressure, and reducing the risk of abnormal heart rhythms. But studies examining the effects of fish oil supplements on various health conditions have produced mixed results.
After reviewing the scientific literature, the AHA released a scientific advisory concluding that omega-3 fish oil supplements may benefit people who have had a heart attack or have documented cardiovascular disease or heart failure. The organization noted, though, that evidence is lacking to support using the supplements to prevent cardiovascular disease in the general population.
One study found that, among 15,480 people with diabetes, daily supplements of 1 gram of omega-3 fatty acids were no better than placebo at reducing major cardiovascular events during a mean follow-up period of 7½ years (New England Journal of Medicine, Aug. 26, 2018). However, a later investigation found that high doses of icosapent ethyl (Vascepa), a prescription form of EPA, significantly reduced the risk of these events (see “Prescription Omega-3 May Lower Cardiovascular Risk”).
One patient population that especially may benefit from fish oil supplements is people with high triglycerides. For those with hypertriglyceridemia, EPA/DHA supplements of 2 to 4 grams a day may be used to reduce triglycerides, but first consult your physician. Several prescription omega-3 supplements are available, as are myriad over-the-counter products.
Caveat Emptor. Any manufacturer who extracts oil from a fish can place the words “fish oil” on a product label, but that doesn’t mean you’ll get what you need from the supplement. In fact, it may be rich in fish blubber and little else. As with any dietary supplement, you need to check the label of your fish oil supplement to make sure it contains adequate amounts of EPA and DHA.
A survey by the U.S. Department of Agriculture found that most omega-3 supplements contained, on average, 180 mg of EPA and 120 mg of DHA per serving. To reduce the number of pills needed to meet recommended omega-3 levels, choose products that contain a total of 600 to 700 mg of EPA and DHA (combined) per capsule.
Also, look for products with the U.S. Pharmacopeia seal, which shows the supplements have been independently reviewed for quality, content, and purity.
Conclusion
Whether you’ve been diagnosed with high cholesterol or you just want to keep it in a normal range, the one thing to remember is that your lifestyle is the biggest factor in improving the health of your heart and blood vessels.
It’s never too late to change your position on the cholesterol continuum—and your heart health—for the better. It’s up to you to follow the diet, exercise, and other lifestyle changes your health-care team recommends. It’s up to you to adhere to the medical treatments your physician prescribes to bring down your cholesterol and reduce your risks.
Stay vigilant and work with your doctor to keep tabs on your lipid levels, blood pressure, and other cardiovascular risk factors. Then, talk with your medical professionals about all your management options.
Use this special report as a guide to help you ask the right questions and gain a better understanding of how you can optimize your cholesterol and your cardiovascular health.
Finding the management approach that’s ideal for you may take some time and effort, but it’s worthwhile. Your heart and arteries will thank you for it.
The post 6. Drug Treatments for Cholesterol appeared first on University Health News.