5. Diseases and Disorders of the Liver
The liver, which is located in the upper-right side of the abdomen, is the largest organ in the body and one of the most important. The liver processes everything you put in your mouth, including food, drink, and medications. It converts nutrients to products the body can use, stores these nutrients, and delivers them where needed. It stores iron, manufactures cholesterol, and makes bile to digest fats. It also removes toxins from the blood, helps maintain regular blood glucose levels, produces immune agents to control infection, and makes proteins that regulate blood clotting.
With so many functions, any disease or disorder of the liver can have a profound impact on the body. In this chapter, we discuss four common liver diseases: hepatitis, cirrhosis, nonalcoholic fatty liver disease, and liver cancer.
Hepatitis
In hepatitis, the liver becomes inflamed. This can be caused by a viral infection or chronic use of medications that can damage the liver, such as acetaminophen (Tylenol). The inflamed liver becomes swollen and tender, and its ability to function properly is impaired. It may become permanently damaged if the infection is not resolved, or use of the offending medication does not stop.
The viruses that can cause the disease are named hepatitis A, B, C, D, and E.
- Hepatitis A is spread by consuming food or water that has been contaminated with human saliva or feces from a person infected with the hepatitis A virus. This is an ongoing problem in parts of the world with poor sanitary conditions. Hepatitis A can also be contracted by close personal contact with an infected person. People at risk for hepatitis A infection include those who travel to parts of the world where hepatitis A is common, children who attend daycare, people who work in a daycare center, and men who have sex with men.
- Hepatitis B can be contracted through contact with the blood, semen, or other body fluid of an infected person. Transmission of the virus can occur through having unprotected sex with an infected person, sharing needles for injecting drugs, sharing toothbrushes or razors with an infected person, receiving a blood transfusion from an infected person, getting a tattoo or body piercing with tools that were not properly cleaned, or getting accidentally pricked with a needle that has contaminated blood on it.
A woman infected with hepatitis B can pass the virus to her baby during childbirth. About 90 percent of these babies become chronically infected, and one in four die. People born in East and Southeast Asia, sub-Saharan Africa, and other areas where the virus is particularly widespread are at high risk for becoming infected, as are people who travel to these areas. Shaking hands and hugging does not pass the virus from person to person.
- Hepatitis C One out of 33 baby boomers (people born between 1945 and 1965) are infected with hepatitis C, although many don’t know it. That’s because most people with hepatitis C have few, if any, symptoms. When symptoms do occur, they can be easily overlooked or attributed to something else, such as the flu. Symptoms generally include jaundice, stomach pain, fatigue, nausea, aching muscles, and loss of appetite. Many people don’t know they have the disease until they develop liver damage many years later.
Hepatitis C is transmitted through contact with the blood or body fluid of an infected person. This can occur due to sharing needles with an infected drug user, being accidentally pricked with an infected needle, or having unprotected sex with an infected person. A mother can pass the virus to her child during childbirth. Anyone who had a blood transfusion or blood product before 1992 is potentially at risk, because blood was not routinely checked for the virus before that date. Patients on long-term kidney dialysis, and those with human immunodeficiency virus (HIV) are also at risk.
- Hepatitis D is transmitted through contact with blood from a person infected with the hepatitis D virus. It only occurs in people who are already infected with hepatitis B.
- Hepatitis E affects about 28 million people worldwide, but is uncommon in the U.S. It is mostly found in Southeast Asia, where it is transmitted by drinking water contaminated with feces from persons infected with the virus.
Hepatitis Symptoms
Hepatitis A, B, and C may cause no symptoms at all, or flu-like symptoms, such as fatigue, nausea, fever, loss of appetite, stomach ache, and diarrhea. Some people experience dark yellow urine, light-colored stools, or yellowish eyes and skin.
Chronic hepatitis B and C take the heaviest toll on Asians, Pacific Islanders, and African-Americans in the U.S. Infection with these viruses account for nearly half of all liver transplants.
Diagnosing Hepatitis
Hepatitis is diagnosed based on the symptoms, a physical exam, blood tests (hepatitis A, B and C), and imaging tests. A liver biopsy also may be taken. In this procedure, a needle is inserted through the skin and into the liver to extract a sample of tissue, which is then analyzed under a microscope.
Treating Hepatitis
Hepatitis treatment depends on which type of the virus is present.
Hepatitis A
Most people who have hepatitis A get better within a few weeks without any treatment. Bed rest and abstention from alcohol are recommended.
Infection with the hepatitis A virus can be prevented with a vaccine. In addition, care should be taken during international travel to avoid drinking tap water and to practice good hygiene. Hands should always be washed after using the toilet and before preparing food.
Hepatitis B
Hepatitis B can last just a short time and resolve on its own without any treatment. However, in some people the infection becomes chronic and can lead to cirrhosis, liver cancer, or death. These people may be treated with an antiviral drug such as interferon, lamivudine (Epivir), adefovir dipivoxil (Hepsera), peginterferon (Peg-Intron, Pegasys), entecavir (Baraclude), telbivudine (Tyzeka) or tenofovir (Viread).
Many patients with hepatitis B may have low levels of vitamin D (see Box 5-1, “Link Between Vitamin D Deficiency and Hepatitis B Seen”). Whether insufficient vitamin D causes hepatitis B, or is the result of it, is not yet known. If a cause-and-effect relationship is established, however, it might be possible to prevent or treat hepatitis B infection with vitamin D supplementation.

A vaccine against hepatitis B has resulted in a large drop in the number of people in the U.S. infected with the virus. The Centers for Disease Control and Prevention (CDC) recommend that children receive their first dose of hepatitis B vaccine at birth and complete the series by six to 18 months of age, and that all children be vaccinated by age 19. All adults should be vaccinated, particularly those at risk.
Using a condom during sex (particularly with a new sexual partner), and avoiding sharing needles, toothbrushes and razors, can help you avoid infection with hepatitis B. If you are getting a tattoo, ensure that a single-use needle in sealed packaging is used, along with single-use disposable inks, and that the tattooist wears a fresh pair of disposable gloves.
Hepatitis C
Hepatitis C may resolve by itself within two to three months. However, in 85 percent of people, the infection slowly becomes chronic, potentially leading to cirrhosis, end-stage liver disease, or liver cancer later in life. Some patients require a liver transplant. About one to five percent of people with hepatitis C die from the consequences of long-term infection. For these reasons, the CDC recommends that all baby boomers be screened for the virus.
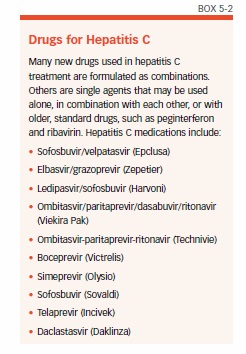
As with hepatitis B, practice safe sex, and avoid sharing needles with other people. Although there is no vaccine for hepatitis C, multiple medications have been developed that increase the chance of cure (see Box 5-2, “Drugs for Hepatitis C”).
Hepatitis D
There is no vaccine for hepatitis D. Chronic hepatitis D is treated with the drug alpha interferon.
Hepatitis E
A hepatitis E vaccine has been developed, but at this time is available only in China.
Cirrhosis
Certain chronic conditions, such as alcoholism and hepatitis, can injure the liver. When this happens, healthy tissue is replaced with scar tissue, resulting in cirrhosis. Cirrhosis prevents blood from flowing smoothly through the liver, so the organ is unable to work properly. About 31,000 people in the U.S. die each year from cirrhosis.
In the U.S., alcoholism is the most common cause of cirrhosis of the liver, which usually only develops after 10 or more years of chronic heavy drinking. Alcohol injures the liver by blocking the normal metabolism of proteins, fats, and carbohydrates. Research suggests that heavy drinkers who are also obese are at even greater risk for cirrhosis.
Chronic infection with hepatitis B, C, or D, and autoimmune diseases can cause inflammation in the liver that, over many years, may lead to cirrhosis (see Box 5-3, “Hope for Patients With Primary Biliary Cirrhosis”). Up to one-fifth of patients with hepatitis C develop cirrhosis. The hepatitis B virus is less common in the U.S., but it is the most common cause of cirrhosis worldwide. Hepatitis D only infects the liver in people with hepatitis B.

Other causes of cirrhosis are rare and include inherited diseases such as alpha-1 antitrypsin deficiency, hemochromatosis, Wilson’s disease, galactosemia, and glycogen storage diseases. In addition, exposure to environmental toxins, the parasitic infection schistosomiasis, heart failure with liver congestion, and adverse reactions to some prescription drugs can also cause cirrhosis.
Cirrhosis Symptoms
In the early stages of cirrhosis, there generally are few, if any, symptoms. As the scarring becomes worse, liver function gradually becomes compromised, and symptoms will start. At first, these may include fatigue, loss of appetite, nausea, weakness, weight loss, abdominal pain, and spider-like blood vessels (spider angiomas) on the skin.
As the disease worsens, the liver becomes more dysfunctional, and complications occur. When the liver can no longer make the protein albumin, water accumulates in the legs (edema) and abdomen (ascites). The liver also makes proteins that are necessary for blood clotting, and without these, the person will bruise and bleed easily. When the liver can no longer absorb bilirubin, the result is yellowing of the skin and eyes (jaundice), and bronzing of the skin. Normally, the liver removes toxins from the blood. If these toxins are not removed, they can build up in the blood and brain, which can affect mental function and memory, and cause personality changes, coma, and even death.
Other complications of cirrhosis of the liver include increased sensitivity to medications, enlarged blood vessels, bleeding veins in the esophagus or upper stomach (varices), insulin resistance, type 2 diabetes, liver cancer, and problems in other organs.
Diagnosing Cirrhosis
Cirrhosis of the liver is usually diagnosed from a combination of symptoms, physical examination, and laboratory tests. During a physical examination, the doctor may detect that the liver feels harder or larger than it should. Blood tests will then be used to measure the levels of certain enzymes that will be present in the blood if the liver has been injured. A CT scan, ultrasound, or MRI of the liver also may be done. The diagnosis can be confirmed with a liver biopsy.
Treating Cirrhosis
The liver damage from cirrhosis is irreversible (see Box 5-4, “Cirrhosis”). For this reason, treatment is directed toward stopping the progression of the disease, and reducing and treating its complications. If fluid accumulation is present (edema or ascites), a low-sodium diet will be recommended, and diuretics may be prescribed. Antibiotics will be used to treat infections, and a diet low in animal protein may help to lower the buildup of toxins in the blood and brain. In severe cases that cannot be controlled, a liver transplant may be necessary.

If cirrhosis of the liver is caused by alcoholism, the first step is to completely abstain from alcohol (in fact, no one who has cirrhosis of the liver, regardless of the cause, should drink alcohol). If cirrhosis is caused by hepatitis, it will need to be treated with medications specific to the type of hepatitis (see Box 5-5, “New Drug Effective in Hepatitis C Cirrhosis”).

Everyone with cirrhosis should eat a healthy diet rich in fruits, vegetables, whole grains, and beans, and low in fat and sodium. Light exercise is also recommended. Because many drugs—both prescription and non-prescription—are processed through the liver, a doctor should be consulted before any medication is taken for any reason.
Nonalcoholic Fatty Liver Diseases
Although alcohol consumption is a common culprit in liver disease, some diseases affect the livers of people who drink little or no alcohol. These include nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH).
NAFLD is a benign condition in which fat infiltrates the liver, but no inflammation or damage occurs (see Box 5-6, “Fatty Liver Disease,” on page 49). Thanks to soaring rates of obesity, NAFLD is the most common liver disorder in the Western world, and affects about 10 percent of children in the U.S. starting at about age two (pediatricians may screen overweight children for the condition). In adults, the condition is usually found during an ultrasound conducted for another reason, such as gallstones.

In NASH, fat is found throughout the liver, along with inflammation and scar tissue. The condition can occur in children as young as 10, and is the primary reason for liver transplantation in children, with poor survival. However, NASH occurs most often in middle-aged adults who are overweight or obese, and have diabetes and insulin resistance. It can also be caused by certain medications and pesticides.
In up to 26 percent of people, NASH progresses to cirrhosis. However, it is not possible to predict how NAFLD will progress in an individual.
NAFLD/NASH Symptoms
Both NAFLD and NASH usually cause few or no symptoms, and are typically detected during a routine blood test for another reason. If liver function tests show abnormalities, the diagnosis of NAFL or NASH must be confirmed with a needle biopsy or ultrasound.
Diagnosing NAFLD/NASH
Blood tests, imaging tests, and liver biopsies may be used to diagnose these conditions.
Treating NAFLD/NASH
There are no accepted medical or surgical treatments for NAFLD or NASH. Clinical trials of various medications and vitamins have included too few participants to draw solid conclusions.
NAFLD is managed with lifestyle modifications that include losing weight, controlling insulin resistance and diabetes, and normalizing blood cholesterol and triglyceride levels. Because the liver is at risk, patients with NAFLD should not drink alcohol, and should be immunized against hepatitis A and B.
For NASH, a diet low in trans fats and fructose (two major components of a fast-food diet), combined with weight loss and increased activity, may help treat the condition. In addition, taking daily vitamin E supplements may reduce fat and inflammation in the liver.
Liver Cancer
Cancer of the liver (see Box 5-7, “Liver Cancer”) is an uncommon but devastating problem affecting about 200,000 U.S. adults every year. No one knows what causes liver cancer, but one study found the highest rates in Texas counties with the highest levels of benzene and toluene in the air. Both chemicals are known to be human carcinogens.

While cancer can start in the liver (primary liver cancer), in the U.S. it more often spreads to the liver from another site (secondary, or metastatic, liver cancer). Most primary liver cancers are hepatocellular carcinomas. Ten to 20 percent are intrahepatic cholangiocarcinomas, or bile duct cancers. Angiosarcoma, hemangiosarcoma, and hepatoblastoma are more rare forms.
Liver Cancer Symptoms
Symptoms of liver cancer frequently don’t manifest until the disease is at a late stage, and include loss of appetite, feeling full after a small meal, nausea and vomiting, abdominal bloating, an enlarged liver and spleen, abdominal pain that may spread to the right shoulder blade, and jaundice.
Diagnosing Liver Cancer
A physical exam may reveal enlargement of the liver or spleen. Imaging tests, such as ultrasound and CT scans, are used to detect masses in the liver and also can be performed to check if liver cancer has spread to other organs.
Treating Liver Cancer
There are multiple treatments for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. These include surgical removal of the lobe of the liver containing the tumor, destroying the tumor without removing it from the body (ablation), cutting off the tumor’s blood supply (embolization), radiation therapy to shrink the tumor, taking medications that target the tumor, and chemotherapy. The best treatment for each patient is based on many factors that include the type of tumor, whether or not it has spread, the patient’s age and overall health, whether or not it is possible to remove the tumor, the likelihood of being cured, and the patient’s feelings about treatment side effects.
Secondary liver cancers are considered extensions of the primary cancer, and are treated as such. Therefore, a liver tumor resulting from lung cancer is treated as lung cancer; a liver tumor resulting from breast cancer is treated as breast cancer.
Chronic hepatitis B and C raise the risk for liver cancer, so practice safe sex, avoid sharing needles with anybody else, and get vaccinated against hepatitis B. Lifestyle factors that increase the risk for liver cancer include excessive alcohol intake (since it raises the risk for cirrhosis), and smoking, so take steps to address these habits if you engage in them. Maintaining a healthy weight also may be protective, since this helps lower the risk for fatty liver disease, which also may raise the risk for liver cancer.
The post 5. Diseases and Disorders of the Liver appeared first on University Health News.
Read Original Article: 5. Diseases and Disorders of the Liver »
Powered by WPeMatico

