7. Treatment
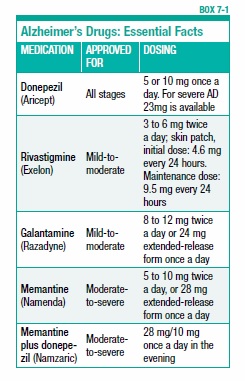
Despite reports of promising new therapies for Alzheimer’s disease, there is still no cure. One or more of the drugs currently being tested may offer hope, but the results of those studies are still a few years away. In the meantime, there are drugs that can treat some of the symptoms. (see Box 7-1, “Alzheimer’s Drugs: Essential Facts”). These drugs may slow the rate of mental decline in many people with Alzheimer’s disease. Mood and behavior symptoms—such as depression, agitation, anxiety, and delusions—can be managed with drugs and other therapies.
Alzheimer’s Disease Drugs
Four main drugs are FDA-approved for Alzheimer’s disease. Three of them—donepezil (Aricept), rivastigmine (Exelon), and galantamine (Razadyne)—are types of drugs called cholinesterase inhibitors. The fourth drug, memantine (Namenda), works by a different mechanism.
Cholinesterase Inhibitors
The plaques and tangles of Alzheimer’s disease cause neurons in the brain to die, resulting in deteriorating brain function. Cholinesterase inhibitors don’t stop neurons from dying. Instead, they help to boost the function of the cells that remain. Brain cells communicate via chemicals called neurotransmitters. Acetylcholine is a neurotransmitter that is depleted in the brains of people with Alzheimer’s disease. Cholinesterase inhibitor drugs stop the enzyme cholinesterase from deactivating acetylcholine. In this way, more acetylcholine remains in the brain for mental functioning.
Studies have shown that cholinesterase inhibitor drugs help about half of people who take them to maintain mental function without significant decline for approximately six months to two years. The drugs are generally considered to be most effective when given in the mild-to-moderate stages of Alzheimer’s disease, but Aricept has also been FDA-approved for use in the later stages of the disease.
Cholinesterase inhibitor drugs can help to maintain brain function for a period of time, but once the function is lost it generally cannot be recovered. Because the drugs can’t prevent neurons from dying, they don’t stop the disease from worsening. And some people are not helped by these drugs at all.
People who do respond to cholinesterase inhibitors generally can retain their current level of memory, language ability, orientation, and attention for a longer period of time than if they were not taking the drugs. The drugs may also have beneficial effects on some behavioral symptoms, such as irritability, anxiety, apathy, and delusions. Studies also have shown that people with Alzheimer’s who take the drugs are better able to handle daily self-care activities, thereby decreasing the amount of time caregivers must spend supervising them. People with Alzheimer’s who take a cholinesterase inhibitor often can remain living at home longer before requiring nursing home care.
People who take these medications should have a positive response within three months. The only way to know if a cholinesterase inhibitor will help is to try it. The potential benefits, risks, costs, and side effects should be discussed beforehand with a doctor.
Aricept and the extended-release form of Razadyne are taken once a day, while Exelon and the short-acting form of Razadyne are taken twice a day. Exelon is also available in a skin patch, changed daily, which releases the drug slowly over time, eliminating the need for twice a day dosing. It also may cause fewer side effects than the pill form.
Side Effects
Potential side effects of cholinesterase inhibitor drugs include nausea, diarrhea, vomiting, fatigue, and weight loss. These tend to be more of a problem at the highest doses of the medications, or if the dosages are raised too quickly. If any of these side effects occur, consult your physician, who may reduce the dose or switch to a different drug.
Memantine for Moderate-to-Severe Alzheimer’s
Memantine works on a different neurotransmitter than the cholinesterase inhibitors, and appears to be helpful for people in the moderate-to-severe stages of Alzheimer’s disease. This distinguishes it from cholinesterase inhibitors, which are useful mainly in the mild-to-moderate stages. Rather than increasing levels of acetylcholine, memantine affects the neurotransmitter glutamate.
Glutamate plays an important role in the parts of the brain responsible for learning and memory. Too little of the neurotransmitter can impair learning and memory, but too much can have damaging effects on brain cells. Alzheimer’s disease may be affected by both too much and too little glutamate at different times.
Memantine protects against excess glutamate and boosts levels of glutamate when they are too low. Possible side effects with memantine include headache, dizziness, confusion, and constipation, although the drug is usually well tolerated.
Because memantine works on a different neurotransmitter than the cholinesterase inhibitors, it can be taken together with one of these drugs. Adding memantine to the drug regimens of patients who were already taking donepezil further improved cognition, ability to perform daily activities, and overall function, according to an analysis of four large studies. Researchers have not tested all of the possible drug combinations. In addition, combination therapy for people in the mild stages of Alzheimer’s has not been adequately tested.
Alternative Treatments
Numerous herbal remedies, vitamins, and dietary supplements are touted as memory enhancers or treatments for Alzheimer’s disease. Some of them may be modestly helpful. Many of them are readily available in drug and health food stores. But keep in mind that the claims about these products may not be based on scientific evidence. Dietary supplements and herbal remedies are not required to undergo the same rigorous study and review as prescription drugs. Therefore, they may not have undergone testing for the desired effect.
Some studies have been conducted to determine whether certain alternative treatments have an impact on Alzheimer’s disease. For many of these the results have been negative or inconclusive. For example, coenzyme Q10 was considered a promising candidate based on studies in mice and in people with Parkinson’s disease. Coenzyme Q10 has not been studied for its effectiveness in treating Alzheimer’s disease—however, a study of a synthetic version of coenzyme Q10 (called idebenone) was conducted in Alzheimer’s patients and found to have no effect.
The herb ginkgo biloba is often marketed as a memory enhancer. It acts as an antioxidant and also increases blood flow by dilating blood vessels. Some small studies suggested that people with Alzheimer’s disease or another form of dementia had improved mental function when taking the herb. However, when ginkgo biloba was subjected to larger, more rigorous studies, it was no more effective than placebo (a sugar pill).
Overall, the evidence that ginkgo biloba improves mental function is weak, and any measurable effect is short lived. In addition, there may be some increased risk of bleeding with ginkgo use.
Antioxidants
Because damage from oxidation caused by potentially harmful molecules called free radicals has been observed in the brains of people with Alzheimer’s disease, researchers have sought to discover whether taking antioxidant vitamins, such as vitamin E, has therapeutic value.
One study showed that patients in the moderate-to-severe stages of Alzheimer’s disease who took 2,000 IU of vitamin E or 10 mg of selegiline (a drug used to control symptoms of Parkinson’s disease) per day for two years were slower to lose their ability to perform basic daily living activities compared to similar patients who took a placebo.
Another study found that for people in earlier stages of Alzheimer’s disease (mild-to-moderate) taking a daily dose of 2,000 IU of vitamin E slowed decline in the ability to engage in normal daily activities, which reduced some of the burden on caregivers.
These studies have caused some doctors to recommend that their Alzheimer’s patients take 1,000 IU of vitamin E twice a day. It should be noted, however, that this is an extremely high dose. Taking such a high dose should be done only under the supervision of a doctor because there are potential adverse effects, such as an increased risk of bleeding.
As more research is conducted, it is important to consult
your physician before taking large doses of any vitamins or
other supplements.
Chinese Herb: Huperzine A
A natural cholinesterase inhibitor, huperzine A has similar properties to the cholinesterase inhibitor drugs donepezil, rivastigmine, and galantamine. Huperzine A, derived from the Chinese herb Huperzia serrata, is available without a prescription and is promoted as a memory enhancer. This herbal supplement has been used in Chinese traditional medicine for centuries, usually as a treatment for swelling, fever, and blood disorders. Chinese researchers have also found it may be useful for Alzheimer’s disease.
Research suggests that this herb has an action similar to cholinesterase inhibitor drugs, which work by maintaining levels of the neurotransmitter acetylcholine in the brain. Acetylcholine is important for learning and memory.
A review of six small trials of huperzine A found that it appears to have some beneficial effects on improving mental function and reducing behavioral problems in people with Alzheimer’s disease, with no obvious side effects. However, a larger trial of huperzine A in individuals with mild-to-moderate Alzheimer’s disease found it was no better than placebo for improving mental function.
Because huperzine A is a natural herb, it doesn’t need FDA approval in order to be sold, and thus the content of the pills you buy is not guaranteed. In addition, since it works on the same mechanism as the cholinesterase inhibitors, they should probably not be used together, as doing so would increase the risk of side effects.
People with Alzheimer’s disease often mirror the emotions of those around them. If caregivers are calm and reassuring, people with dementia will pick up on that, and this may help them remain calm as well.
Cognitive Rehabilitation
It’s often thought that damage to memory and learning systems in the brains of people with Alzheimer’s disease makes it almost impossible to form new memories and learn new information. However, people in the early stage of the Alzheimer’s can still learn, and this ability can be enhanced with cognitive rehabilitation techniques. These techniques can help teach people how to recall important information and to perform better in daily tasks.
Rehabilitation programs may involve learning face-name recognition techniques, getting memory notebooks in which to record appointments and schedules, and learning ways to improve financial skills.
One study showed that people in the early stage of Alzheimer’s disease who participated in a cognitive rehabilitation program were able to retain implicit memories as well as younger adults and older adults without dementia. Implicit memory is the unconscious memory for common skills and activities, such as speaking a language or riding a bicycle.
Cognitive rehabilitation has traditionally been used to help people who’ve had strokes or suffered traumatic brain injuries recover cognitive functions and improve memory. Its use for Alzheimer’s disease is relatively new, but the positive results from studies show that people in the early stages of Alzheimer’s disease can still learn, and this ability can be enhanced with cognitive rehabilitation techniques.
Treating Behavioral Symptoms
In addition to cognitive symptoms, people with Alzheimer’s disease may exhibit behavioral symptoms, including anxiety, agitation, aggression, apathy, depression, delusions, and hallucinations. Drugs may help with some of these symptoms, but they are not always effective and can have undesirable side effects. Before medication is used, caregivers should try non-drug strategies.
Recent evidence shows that physical exercise may help calm agitated behaviors in people with mild-to-moderate Alzheimer’s disease. In a study of 200 people with Alzheimer’s disease, those who participated in an aerobic exercise program for one hour three times a week for 16 weeks had a reduction in psychiatric symptoms, such as anxiety, irritability, and depression.
Non-Drug Strategies
Changes in behavior often have specific causes, such as physical discomfort or pain that cannot be expressed, fear of unfamiliar surroundings and loud noises, frustration from trying to communicate with others, and annoyance at the inability to take care of household tasks and personal grooming. Moving to an assisted living facility or nursing home can cause agitation and other behavioral problems, as can changes in caregiver arrangements.
A person with Alzheimer’s disease may be unable to describe specific physical complaints. Therefore, physical discomfort may be expressed as agitation. Look for evidence of common physical discomforts, such as pain, hunger, constipation, urinary tract infection, pneumonia, skin infection, or bone fracture. If present, these conditions should be appropriately treated.
New medical conditions or medications may also be sources of behavioral symptoms. For example, new or worsening vision or hearing problems can cause confusion or frustration. Many older adults, including those with Alzheimer’s disease, take one or more prescription drugs for other health problems. Side effects from these drugs may affect behavior. When a new behavioral symptom occurs, look for a medical cause. A visit to the primary care doctor is recommended.
Once medical conditions have been addressed, there are other effective non-drug strategies that may help with some behavioral problems. For example, consistency in the home environment is important. The home should be arranged to reduce confusion, disorientation, and agitation. Lighting and noise levels should be adjusted to provide a calm environment (the lights shouldn’t be so dim that they cause problems for people with low vision, however). Loud and erratic noises should be avoided. To make the home feel safe and to reduce anxiety, don’t rearrange furniture or make any other drastic changes. Keep personal possessions, including favorite photographs, in visible locations, and don’t move them around.
Handling Agitation, Irritability, and Aggression
Caregivers can often lessen agitation, irritability, and aggression in a person with Alzheimer’s disease by learning what to expect and how to communicate effectively. Sometimes breaking down a task into its component parts can decrease frustration and help the person to be more self-sufficient. For example, if a person with Alzheimer’s disease gets agitated when asked to brush his teeth, break down the task into smaller directions. Say: “Take the toothbrush.” “Put it under the water.” “Here’s the toothpaste.” “Put the brush in your mouth.” “OK, now you can brush.”
Sometimes, the best remedy for agitation is gentle reassurance from a compassionate caregiver. People with Alzheimer’s disease often mirror the emotions of those around them. If the caregiver becomes angry, agitated, or impatient, the person with dementia may pick up on these emotions and express them. If the caregiver is calm and reassuring, the person with dementia will pick up on that, and this may help.
Caregivers should help people with Alzheimer’s disease plan activities, keep a schedule, and organize their time. Keeping the person involved in household and personal care activities for as long as possible may lessen feelings of helplessness and dependence. It’s also important not to neglect leisure activities, such as music, painting, walking, or reading. Planning activities—both household and recreational—around a set schedule may help to relieve agitation.
Get Support
Counseling and support groups are valuable resources for caregivers to discuss specific behaviors and get advice on how to handle them. The Alzheimer’s Association has chapters across the United States that offer assistance and support groups, as well as a 24-hour helpline (see Appendix II: Resources, page 96).
Drug Treatment
If non-drug strategies are not effective and symptoms of depression, anxiety, agitation, sleeplessness, and aggression are severe, a doctor may prescribe medications. Although there are no FDA-approved medications specifically for the indication of behavioral disturbance from dementia, doctors have found that a variety of medications can be helpful to patients with these problems.
Antidepressants are designed to treat depression. The antidepressants most commonly used for older persons with dementia are from a group known as selective serotonin reuptake inhibitors (SSRIs), such as sertraline (Zoloft) or citalopram (Celexa). These drugs have relatively few side effects and are taken once a day. If they don’t work, there are many other antidepressant drugs for the physician to choose from.
Anti-anxiety drugs may be used to relieve anxiety and help the person sleep. These include lorazepam (Ativan) and oxazepam (Serax). Drugs may be given over the short term to calm a person down during a crisis, or they may be given as needed for longer periods to deal with more persistent problems. All of the drugs used for behavioral symptoms have benefits and potential side effects, including an increased risk for falling, and patients who are taking them need to be carefully monitored.
Antipsychotic drugs are sometimes used to treat agitation, hallucinations, and delusions in people with Alzheimer’s disease. These drugs may be helpful for some people in certain circumstances, but they must be used with extreme caution. Some of the antipsychotic drugs can cause side effects, such as sedation, confusion, and weight gain. In addition, all antipsychotics may increase the risk for death among people with dementia. The FDA has issued a warning about this possibility.
Antipsychotics may be appropriate for some people in some circumstances. For example, they may be effective for people with severe agitation. Antipsychotic drugs should most likely be used only as a last resort, and for the shortest possible time at the lowest possible dose. They should not be used to sedate or restrain a person.
It may take several attempts to find the right drug, or combination of drugs, that are most helpful. Even if drugs are used for behavioral symptoms, it is important to continue using non-drug approaches to calm agitated and irritable behavior.
The post 7. Treatment appeared first on University Health News.
Read Original Article: 7. Treatment »
Powered by WPeMatico