Heart Arteries Aren’t the Only Ones That May Be Clogged
Peripheral artery disease (PAD) is a buildup of plaque within the peripheral arteries in the legs and arms. It may not sound as serious as coronary artery disease, since it doesn’t occur in or around the heart, but it can have serious consequences if it’s not diagnosed and treated. A diagnosis of PAD can also alert you to the likelihood of plaque buildup in other areas of your body, including your heart.
“PAD is very common; an estimated 8 to 12 million people are affected in the U.S, and approximately one in every 20 Americans over the age of 50 has PAD,” explains Dmitriy Feldman, MD, FACC, director of endovascular services and an associate professor of medicine at Weill Cornell Medicine. “It is important to know if you have PAD, because the presence of PAD signifies a future risk for having a heart attack or a stroke.”
The risk of having PAD increases with age, current or prior smoking, diabetes, obesity, high blood pressure, and high total and LDL cholesterol levels— the same risk factors that increase the chances of coronary artery disease.
Be Alert for Symptoms
PAD most commonly affects arteries in the legs. According to Dr. Feldman, symptoms include cramping in the lower extremities and/or pain or tiredness in the calf or hip muscles, particularly when walking or climbing stairs. In more advanced stages of PAD, symptoms include sores or wounds on the toes, feet or legs, a lower temperature in the extremity, color changes in the skin of the toes and/or feet, and poor nail growth or hair growth on the toes and legs, respectively.
“It’s important to know if you have PAD because the loss of circulation to the legs and feet can cause gangrene and loss of a limb,” says Dr. Feldman. PAD can be present without any symptoms, so people can have PAD and not know about it. PAD can also be present in the arteries that carry circulation to the brain, arms, kidneys, and stomach.
Diagnosing PAD
Dr. Feldman notes that PAD can be easily diagnosed with an evaluation that includes a thorough medical history, a physical exam, and diagnostic tests. The evaluation can be performed by the patient’s primary care physician, or by doctors who specialize in the diagnosis and treatment of PAD, such as cardiologists, vascular medicine specialists, surgeons, and podiatrists. An evaluation for PAD usually includes a simple, noninvasive, diagnostic test called an ankle-brachial index (ABI). This test compares the blood pressure readings in your ankles with the blood pressure in your arms; if the pressure in your ankles is significantly lower than in your arms, you probably have PAD. Dr. Feldman says that further tests, such as Doppler ultrasound of the arteries in the lower extremities, a magnetic resonance angiography, or a computerized tomography angiography, may be needed to identify the location and severity of the blockages.
Treatment Options
The goal of treating PAD is to improve quality of life, alleviate symptoms, and reduce the chances of heart attack, stroke, or amputation. Dr. Feldman explains that there are three main treatment approaches to PAD, which include:
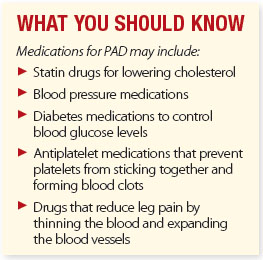
- Medications and lifestyle changes (treatment of hypertension, diabetes, and/or cholesterol, eating a healthy diet, getting regular exercise, and weight loss and smoking cessation, if required)
- Minimally invasive endovascular procedures, including balloon angioplasty (this involves threading a catheter with a balloon on the tip to the narrowed or blocked artery and inflating the balloon, which increases blood flow) or stenting (a small, hollow mesh tube called a stent is threaded to the site of the blockage and placed there, holding the artery open)
- Bypass graft surgery, in which a blood vessel from another section of your body is attached to the artery on either side of the blockage, allowing the blood to flow around the area that is blocked.
“Many cases of PAD can be treated with lifestyle changes, an exercise program, and medications,” says Dr. Feldman. “If the blood flow in the extremities is severely reduced and causing severe symptoms, patients may benefit from procedures that include angioplasty with drug-coated balloons, stenting, atherectomy (removal of plaque from the artery), or a surgical intervention.”
The post Heart Arteries Aren’t the Only Ones That May Be Clogged appeared first on University Health News.
Read Original Article: Heart Arteries Aren’t the Only Ones That May Be Clogged »
