Carotid Artery Disease Raises Stroke Risk
One of the main risk factors for stroke is atherosclerosis, a condition that develops when cholesterol and other fatty substances build up in the inner lining of arteries and form deposits called “plaques.” When atherosclerosis affects the carotid arteries (the main arteries to the brain), the condition is known as carotid artery disease. “Carotid artery disease is more likely to occur in older adults because age makes arteries less flexible and more susceptible to damage,” explains Kara F. Sheinart, MD, assistant clinical professor of neurology at Mount Sinai. “Having a family history of carotid artery disease or other vascular disease also makes you vulnerable. However, some risk factors for carotid artery disease are modifiable, and the condition also can be effectively treated.”
Reduced Blood Flow The carotid arteries are situated on each side of the neck, and each of them branches to form internal and external arteries. The internal arteries supply the brain with oxygen-rich blood, while the external arteries supply the face, scalp, and neck. But the flow of blood can be impeded if atherosclerosis narrows the carotid arteries (known as carotid artery stenosis). “In the short term, other arteries expand to try to compensate,” Dr. Sheinart says. “However, over time, the reduced blood supply can block the flow of blood to the brain, putting brain cells at risk of damage from lack of oxygen. It also is possible for a fragment of the cholesterol plaque to break loose and travel to the small blood vessels of the brain through one of the internal carotid branch arteries.” This may result in a stroke or a transient ischemic attack (TIA), which can precede a stroke.
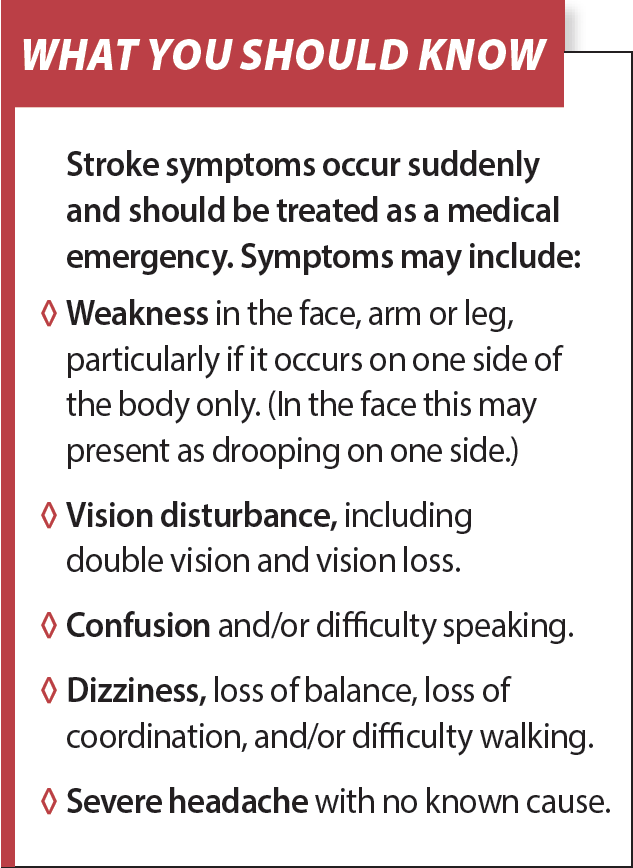
Routine Screening Not Recommended Despite its link with stroke, carotid artery disease is not routinely screened for in people without multiple risk factors for the condition and those who are not experiencing symptoms suggestive of a TIA or stroke (see What You Should Know for warning signs). In a recent statement (Journal of the American Medical Association, Feb. 2), the U.S. Preventive Services Task Force reaffirmed that routine screening is not advisable, pointing to evidence that the harms of screening outweigh its benefits. “Possible harms include false positive results that cause people anxiety and may result in unnecessary and potentially risky additional tests and surgical procedures in people who don’t really need them,” Dr. Sheinart says.
Diagnosing Carotid Artery Disease Carotid artery disease typically doesn’t cause symptoms in its early stages. However, in some people it causes a “bruit” (a whooshing sound that signals reduced blood flow in the arteries), so if you have carotid artery disease risk factors, your doctor may periodically listen to your carotid arteries with a stethoscope to check for a bruit. (Note that carotid artery disease does not always cause a bruit.)
If you have symptoms suggestive of a TIA or stroke, your doctor may recommend screening using carotid ultrasound or carotid Doppler ultrasound. “Standard ultrasound uses sound waves to create an image of the inside of the arteries, while Doppler ultrasound also evaluates how well blood is flowing through the arteries,” says Dr. Sheinart. If necessary, magnetic resonance angiography or computed tomographic angiography also may be ordered to further clarify the degree of carotid stenosis. Both tests may involve having a contrast dye injected into a vein—the dye travels to your carotid arteries and x-rays are taken as it passes through them to ascertain whether they are narrowed or blocked.
Treating Carotid Artery Disease Drugs are the mainstay when it comes to treating mild to moderate carotid artery disease. You already may be taking cholesterol-lowering statins and blood pressure drugs, but you also may need to start taking anti-platelet medications. These prevent platelets (small cell fragments that circulate in the blood and form clots to prevent bleeding) from clumping together—options include aspirin and clopidogrel (Plavix®).
If your carotid artery disease is severe, or you already have had a TIA or stroke, your doctor may recommend carotid endarterectomy or stenting. Which is best for you depends on your age and overall health, and the location of the cholesterol plaque.
- In carotid endarterectomy, the carotid artery is accessed surgically via an incision in the neck and the cholesterol plaque is removed. “In some cases, the artery wall may need to be reinforced with a synthetic patch or a graft taken from one of your leg veins,” says Dr. Sheinart. “The procedure typically takes less than two hours, and you can expect to stay overnight in the hospital afterward. Most people are able to resume normal activities within a few days, but you’ll need to take daily low-dose aspirin afterward.”
- Carotid stenting involves having a balloon-tipped catheter carrying a tiny mesh tube inserted into an artery in your arm or leg. “The catheter is threaded to the blockage in the carotid artery, whereupon the balloon tip is inflated to compress the cholesterol plaque against the artery walls and position the stent,” Dr. Sheinart explains. “The catheter is then withdrawn, leaving the stent in place to keep the artery open.” The procedure takes about two hours, and you may need to lie still for several hours afterward to prevent the catheter insertion site from opening up and bleeding. “Most people go home the following day,” Dr. Sheinart says. “It is necessary to take clopidogrel and low-dose aspirin daily for at least one month after the procedure, and continue aspirin daily thereafter.”
Both carotid endarterectomy and stenting have been shown to prevent TIAs and strokes in selected individuals. “However, as with any surgery or procedure, they are associated with a risk of complications, including bleeding, infection, stroke, heart attack, and death,” Dr. Sheinart says. Complications are more likely in people age 75 and older, and in those who have severe heart or lung disease, heart failure, or diabetes. “The risk of complications means it’s vital to consult a doctor with experience in carotid artery endarterectomy and stenting,” Dr. Sheinart emphasizes. “He or she can thoroughly evaluate your suitability for these procedures.”
Preventing Carotid Artery Disease A TIA or stroke may be the first sign that you have carotid artery disease, so take steps to tackle the modifiable risk factors that make you more vulnerable to atherosclerosis. These include high blood pressure, cholesterol and blood sugar, obesity, lack of exercise, and tobacco use.
If you’re taking medications to control high blood pressure, cholesterol and blood sugar, be sure to follow your doctor’s guidance on how much medication to take and when. Also be guided by your doctor on lifestyle approaches that may help you control these risk factors as well as manage your weight. Aim to eat a healthful diet rich in fruits, vegetables, whole grains and fatty fish (such as salmon, sardines and trout), get at least 30 minutes of physical activity each day (brisk walking is ideal), and quit smoking if you engage in the habit. (See our February issue for smoking cessation strategies.)
Seek Help Fast for Stroke Swift treatment with clot-busting medication may help prevent severe complications after stroke. However, for the best results, the drug needs to be administered within four to five hours of stroke onset. If you experience symptoms that may indicate a stroke, call 911 and get to an emergency room as quickly as possible.
The post Carotid Artery Disease Raises Stroke Risk appeared first on University Health News.
Read Original Article: Carotid Artery Disease Raises Stroke Risk »

