Modifiable Lifestyle Habits Are Central to New A-fib Guideline
An updated atrial fibrillation (A-fib) treatment guideline redefines how the disease should be managed and prevented, stressing the importance of lifestyle modifications. Developed by a panel of cardiologists in conjunction with the American Heart Association and the American College of Cardiology, the treatment recommendations reflect a change in how A-fib is now viewed by experts in the cardiovascular field. Read on to learn what that means for women who have A-fib, as well as those who are at risk for the disease.
Historically, patients who had A-fib were evaluated and managed based solely on the duration of the irregular heartbeat that is A-fib’s primary symptom. Now, the guideline emphasizes that A-fib requires a variety of strategies at its different stages—from prevention to therapeutic treatment—with an emphasis on modifiable lifestyle habits such as exercise, diet, and reduced alcohol consumption.
Recognizing A-fib
A-fib, is the result of irregular beating of the heart’s upper chambers. It leads to disrupted blood flow and an increased risk of stroke, heart attack, and heart failure. A-fib manifests as heart palpitations or irregular heartbeat, sometimes accompanied by other symptoms, including lightheadedness, fatigue, chest pain, and shortness of breath. It is the most prevalent heart rhythm disorder, and its incidence is growing. The American Heart Association estimates that there are 50 million people worldwide who have A-fib. The prevalence of A-fib increases with age, and is more common in women than men. What’s more, “Women are more symptomatic and report worse quality of life with A-fib and are at higher risk of stroke,” says Jessica M. Peña, MD, Weill Cornell Medicine, Director, HeartHealth, Dalio Institute of Cardiovascular Imaging.
Preventing and Managing A-fib
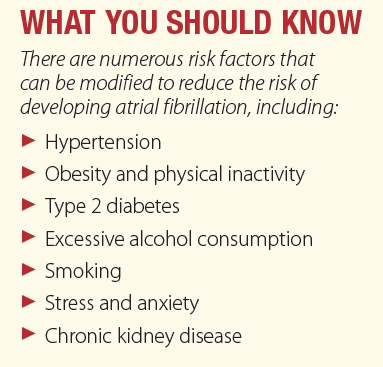
Making lifestyle changes and tweaking other modifiable risk factors to prevent onset, progression, and adverse outcomes of A-fib are the backbone of the guideline. “While advising patients to improve modifiable risk factors has always been part of A-fib management, the new guideline is more focused on this aspect. For example, the guideline specifies the amount of exercise recommended to reduce the burden of A-fib, and also advocates for 10 percent weight loss in individuals with A-fib who have obesity or are overweight,” says Dr. Peña. The guideline states that moderate-to-vigorous exercise for 210 minutes per week has been shown to reduce A-fib symptoms.
Reassessing Anticoagulation
The guideline reassesses the role of anticoagulation therapy, which plays a key role in A-fib management. A-fib is associated with an increased risk of blood clots, which can lead to stroke, and anticoagulants help prevent the formation of blood clots. The guideline suggests that doctors use a “risk score” calculation to gauge how likely it is that someone will develop a blood clot, and then base their use of anticoagulation medicine on the score. Because anticoagulant therapy carries a risk of bleeding, it can be especially concerning for people with a high risk of bleeding due to factors such as advanced age, history of gastrointestinal bleeding, or use of medications that increase the risk of bleeding, such as aspirin and non-steroidal anti-inflammatories. “The decision to start or continue anticoagulation takes into account a person’s risk of stroke and bleeding, as well as their preferences and other risk factors,” says Dr. Peña.
Catheter Ablation
The guideline includes recommendations for changing how and when people seek certain treatment options. An example is catheter ablation. This is now considered a reasonable first-line treatment for A-fib. The surgery, which takes from two to four hours, entails having an electrophysiologist—a specific kind of cardiologist—perform a procedure that blocks irregular electrical signals within the heart to reduce arrhythmia episodes. According to the guideline, scientific evidence shows that ablation is superior to any available antiarrhythmic drug.
The guideline underscores the need for a comprehensive and proactive approach to patient care, integrating treatment with lifestyle interventions. “By taking proactive measures including lifestyle changes, risk management, early catheter ablation, and stroke risk reduction, we can prevent, detect and manage A-fib and its consequences,” says Dr. Peña.
The post Modifiable Lifestyle Habits Are Central to New A-fib Guideline appeared first on University Health News.
Read Original Article: Modifiable Lifestyle Habits Are Central to New A-fib Guideline »

