Insights into Hip and Knee Replacement
When looking for a good joint replacement surgeon, you might not think to include expertise in revision surgery as part of your search criteria. After all, you expect the surgeon to get it right the first time. The good news is that about 95% of hip replacement surgeries are very successful and help people lead more active, pain-free lives. But according to a 2017 report in The Lancet, 4 to 5% of people who receive a total hip or knee replacement may require revision surgery within 10 years. There are many reasons why this may be necessary. For example, wear and tear of the implants, infections, loosening of the implants over time, or misalignment of implants during the primary (first) surgery.
In this candid conversation about joint replacements, UCLA Health orthopaedic surgeon Adam Sassoon MD, explains why you want a surgeon who does revision arthroplasty as well as primary surgeries. He also shares other insights that can help you have informed conversations with physicians.
Surgeon Insights
“Doctors don’t like to talk about complications, and they don’t happen routinely, but they can happen,” says Dr. Sassoon. “When they do, you want a doctor who can manage any problem. There are lot of surgeons who refuse to do revision work. I think that’s unfortunate because if you’re one of their patients and you have problems, you must find another provider. Patients should choose a surgeon that is fellowship trained, which means that in addition to their residency, they’ve completed an additional year of specialty training in a hip and knee replacement. You should also choose a surgeon that offers both primary and revision surgery.”
UCLA Medical Center is a referral center, and greater than 95% of the revision surgeries Dr. Sassoon does are on people who had their procedure somewhere else.
Deciding When It’s Time
It’s no secret that hip and knee pain can get in the way of having fun or just doing simple daily activities. To address the pain, many people have freezers filled with ice packs, use compression sleeves or knee braces, and take anti-inflammatories. Some people have had physical therapy and perhaps have tried joint injections. If those all of those have failed, it’s time to seriously consider joint replacement.
If you think you’re too old, know that there’s no age limit for joint replacement surgery. Dr. Sassoon’s oldest patient was 102. It’s not about age, but rather when the joint was destroyed and how it interferes with your quality of life. For example, joint replacement is a viable option when hip or knee pain is preventing you from activities that make you happy and/or is interfering with biological functions, such as getting a good night’s sleep, having sex, or getting on and off the toilet. “Once it’s impacting your life in those ways and you’ve tried and failed other treatments, then it’s time for joint surgery.”
Not long ago, Dr. Sassoon performed a double knee replacement on 76-year-old Robert Lombard, who started surfing at the age of 62. The tipping point for Lombard was when the pain of arthritis was keeping him from his beloved, spiritually enriching sport. Nonetheless, he was understandably nervous about the procedures. Dr. Sassoon knew he could make it better and promised to surf with him after he recovered. Lombard had his right knee operation in July 2021 and the left done in November 2021. On April 17, 2022, they were catching waves in Huntington Beach, California.
Procedural Insights
There are numerous ways to effectively perform hip and knee procedures. For hip replacements, Dr. Sassoon prefers using accelerometry-guided navigation tools. Unlike large robotic counsels, accelerometry-guided navigation uses a handheld device that doesn’t require as many pins and incisions. Some robotic systems confine surgeons to a particular implant manufacturer. “The accelerometry-guided method is faster than traditional robotics. It doesn’t require pin tracks, or preop imaging, and I can use any implant system that I feel is right for the patient,” he explains.
Total hip replacement involves cutting off arthritic bone, removing damaged cartilage, and replacing those parts with implants.
But that’s not the case with knee replacement. “Many people think we’re going to remove their joint, but we’re just shaving off the diseased portions of the joint and putting a cap on it,” he explains. “It’s kind of like a crown for a tooth.”
Compared to the hip, the knee is a much more complicated joint. The complexity makes for a more difficult recovery. But on the positive side, because the knee has several compartments, it’s possible that only one part may need surgical intervention, sparing the rest of the joint. The compartments include the medial portion (inner knee toward the midline of the body), the lateral (outer part) and the patellofemoral (inside behind the kneecap). Compared to total knee replacement, partial replacement is faster, recovery is quicker, and the risk of complication is lower.
“Many surgeons don’t do partial knee replacements,” says Dr. Sassoon. “You have to do a lot of them to have good results.”
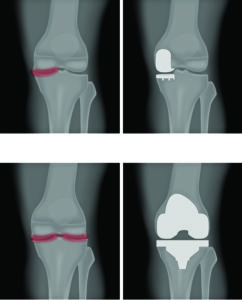
Partial Knee Replacement (top)
Total Knee Replacement (bottom)
© Aksanakulchytskaya | Dreamstime
Patellofemoral arthritis affects just the cartilage behind the kneecap and causes an instability in the joint. It causes pain in the front of the knee and makes it difficult to squat and go up and down stairs. To successfully address this problem, the soft tissue needs realignment along with partial knee repair. Dr. Sassoon and UCLA orthopaedic surgeon Kristofer Jones (team doctor for the L.A. Lakers) collaborate to address this unique problem. Dr. Jones realigns the soft tissue and Dr. Sassoon resurfaces the kneecap and inserts replacement parts as needed. For a more detailed explanation about this procedure and others, go to laorthosurgeon.com.

The Value of High Volume
No matter what, if you’re having any kind of joint replacement, you’re better off in the hands of a surgeon who does a high volume. One study found that the need for revision surgery to correct a problem with the initial surgery was 22% higher among surgeons who do fewer than 12 hip replacements per year, compared with those who did more. Regarding partial knee replacements, “a lot” is defined as at least 30 partials per year. Dr. Sassoon does about 40 to 50 per year.
Rehab and Recovery
Because the hip joint is not as complex as the knee, many patients may not need formal physical therapy after hip replacement. “We give them a home exercise program. They also start walking with a walker, transition to a cane and then graduate from gait aids entirely,” explains Dr. Sassoon. “For knee replacements, I prescribe outpatient physical therapy on day two or three after the procedure. With knees, you’re fighting against postoperative stiffness; you must aggressively stretch the knee to keep the joint supple. That requires more formal physical therapy and more encouragement because the stretching does hurt.”
In general, after joint replacement people can return to daily life activities (though not demanding or high- impact sports) after about six to eight weeks. Most knee and hip procedures are done without general anesthesia; instead regional anesthesia (e.g., short-acting spinal block) is used. That facilitates the opportunity for many people to have these procedures as outpatients. Most joint replacements at UCLA are done this way. Having good support at home is key.
Total joint replacements for hips can last 30 years or more, and knee replacements can last 20 years or longer. Given the many benefits of physical activity, it’s a worthwhile procedure available to most people.
The post Insights into Hip and Knee Replacement appeared first on University Health News.
Read Original Article: Insights into Hip and Knee Replacement »

