Drug-Free Strategies to Ease Your Aching Head
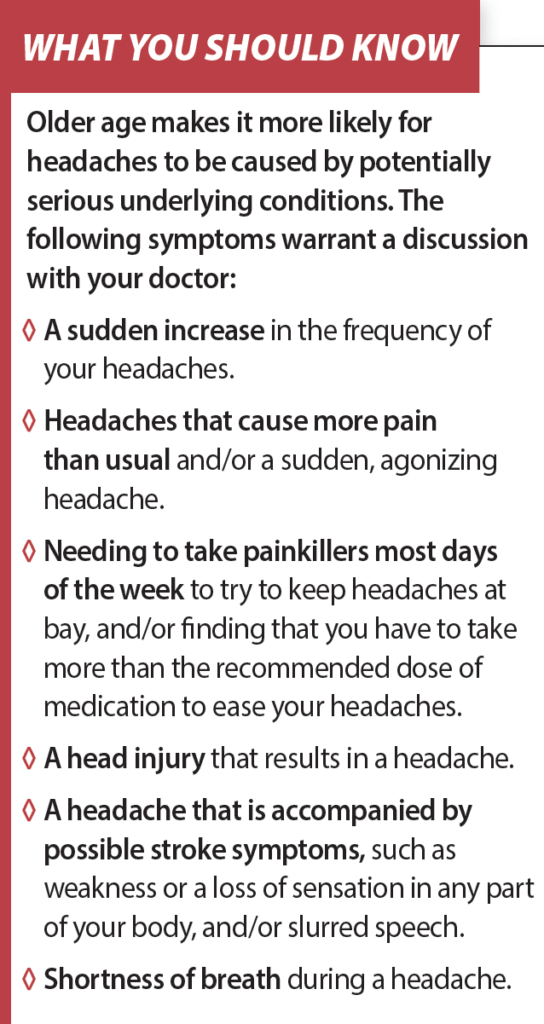
While you may have heard that older adults are less likely than their younger counterparts to suffer from headaches, the problem does continue past age 65. Usually they don’t signal anything serious—however, if they worsen you should tell your doctor. “It’s also important to alert your doctor about new-onset headaches, headaches that develop after a head injury, and headaches that are accompanied by signs that may indicate a stroke,” says Mount Sinai geriatrician Patricia Bloom, MD. See What You Should Know, on the bottom of this page, for more headache red flags.
Tension Headaches Most Common Tension headaches are the most likely type to persist in older age. “They are thought to result from a combination of having a heightened sensitivity to pain and a tendency to subconsciously tighten the muscles of your face, neck and shoulders in response to stress,” says Dr. Bloom “They affect both sides of the head, and feel like constant pressure or squeezing, unlike the one-sided pulsing, throbbing pain that characterizes more severe headache disorders, like migraines and cluster headaches.”
Tension headaches can become harder to manage as you age if you’ve been relying on over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil®, Motrin®) or naproxen (Aleve®) to ease the ache. NSAIDs are effective but they are
associated with serious side effects, including a raised risk of gastrointestinal (GI) issues like ulcers, and bleeding, in older adults. Acetaminophen (Tylenol®) is considered safer for older adults, but can damage your liver if you inadvertently overdose on it. The usual daily limit for acetaminophen in younger people is 4,000 milligrams (mg), which is equivalent to eight 500 mg tablets. “However, older adults should limit themselves to 3,000 mg, or six 500 mg tablets,” Dr. Bloom says. “It’s also important to factor in other medications that contain acetaminophen, such as over-the-counter cold and flu remedies. Avoid using these if you’re also taking acetaminophen tablets.”
Rebound Risk Acetaminophen also raises the risk of rebound headaches if you regularly take it to treat tension headaches. These headaches typically strike in the morning, when painkillers you took the day before have worn off. The only way to stop rebound headaches from occurring is to cut back on your usual painkilling medications. To help ease your headaches while you do so, try the following non-drug pain-relief strategies. These approaches also may provide some relief from migraines; however, it is likely you will still need to take medications to help you manage these more severe headaches when they strike.
- Give Yourself an Acupressure Massage Use your fingertips to apply pressure to these areas of your face (one minute for each area): the area between your eyebrows; just above the inner corner of each eye and below your eyebrow; the area above the top of your ears; each side of your nostrils; each side of the back of your neck; and the tops of the shoulders. “Other acupressure spots that may help headaches include the skin between the base of your thumb and the base of your forefinger,” Dr. Bloom adds.
- Try Aromatherapy This involves inhaling or applying essential oils from plants (the oils should not be ingested). You can easily inhale the oils by sprinkling a few drops onto a tissue or into a bowl of hot water, but if you’re using the oils topically, take precautions. “Essential oils are very concentrated and should be diluted in a carrier oil, such as sweet almond oil, if you intend using them topically,” Dr. Bloom advises. Mix three drops of peppermint essential oil or lavender oil in a teaspoon of carrier oil and use it to massage your temples. Other essential oils that may benefit headaches include chamomile, eucalyptus, and thyme.
- Meditate Meditation can help distract you from pain and stress. “You can meditate by sitting in a quiet room with your eyes closed, regulating your breathing, and being conscious of the sound of your breath as you inhale and exhale,” Dr. Bloom says. “Many people report that a chant such as ‘ohm’ is helpful to drain away tension.” There are many guided meditations available online—you also might want to download a smartphone meditation app, like Headspace or Calm.
- Sip Ginger Tea Ginger is believed to reduce inflammation in the blood vessels of the head. You can make ginger tea by bringing a small amount of sliced ginger root to boil in two cups of water. Simmer the mixture for about 30 minutes and allow it to cool to warm before you drink it.
- Curb the Caffeine Too much caffeine can cause or worsen tension headaches, but if you’re a regular coffee drinker, stopping cold turkey also can cause a headache. “Try to keep your coffee intake to one or two cups a day, and if you currently have more than this, cut back gradually by switching to half-caf,” Dr. Bloom says. “Many soft drinks also contain caffeine, so watch your intake of these.”
- Get Enough Fluids Dehydration can contribute to tension headaches and migraines. “As you age, your thirst sensation tends to wane, so you shouldn’t rely on feeling thirsty to signal that you need to rehydrate,” Dr. Bloom says. “Eight glasses of water a day is a good general target for fluid intake, but remember you can also factor in fluids contained in foods.” Soup is an obvious example, and some fruits and vegetables are high in water—examples include watermelon, grapefruits, and lettuce.
- Tackle TMJD This stands for temporomandibular joint disorder, which is typically accompanied by frequent tension headaches. The condition tends to be more common in people who clench or grind their teeth, and in those who have arthritis. Symptoms include a popping, clicking and/or grating sound when you open your mouth wide (for example, when yawning or during a dental exam). If you have TMJD, wearing a simple bite-guard at night can help—ask your dentist about having one fitted.
- Perfect Your Posture If you tend to slouch, it’s likely that your head juts forward and pulls on the muscles in your neck, shoulders, and upper back. Not only can this contribute to tension headaches and migraines, it also can result in upper back pain. “Try to keep your head lined up between your shoulders, and your shoulders lined up with your hips,” Dr. Bloom advises. “The best way to do this is to imagine an invisible string is attached to the top of your head, pulling it slightly backward and up.” If you’re struggling to stay aligned, consider taking classes in the Alexander technique, an exercise method that improves posture and coordination. The American Society for the Alexander Technique (www.amsatonline.org) has a register of local teachers.
The post Drug-Free Strategies to Ease Your Aching Head appeared first on University Health News.
Read Original Article: Drug-Free Strategies to Ease Your Aching Head »