3. Diagnosing COPD
COPD and asthma share many of the same symptoms (primarily coughing, wheezing, and shortness of breath), which occur because normal airflow into and out of the lungs is obstructed. This can make it difficult to distinguish between the two conditions, especially in middle- and older-aged adults with a history of smoking. Regardless of the age that these symptoms first appear, it’s important to make an accurate diagnosis, because treatment often differs for the two conditions.
The first step is to perform a physical examination, take a detailed medical history, ask about smoking (in adults) and other lifestyle issues, and perform diagnostic tests.
COPD is suspected in anyone with a history of smoking or exposure to environmental irritants who has any of the characteristic symptoms of COPD.
In a patient with symptoms of COPD, or a history of exposure to risk factors for COPD (such as cigarette smoke), spirometry is used to make the diagnosis. It is also used to assess the severity of COPD.
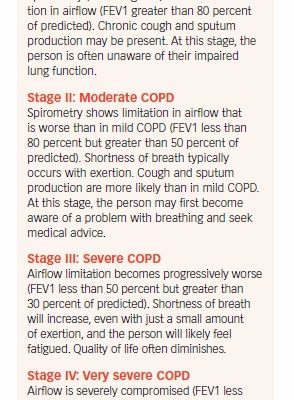
Using the spirometry reading, a patient’s COPD is classified by stage: mild, moderate, severe, and very severe (see Box 3-1, “Stages of COPD”). These classifications are based on increasing severity of airflow restriction and symptoms.
In someone with COPD, the amount of air that can be blown out in one second (FEV 1) drops. As the disease worsens, the total amount of air that can be exhaled after inhalation (FVC) also drops.

Tests Used to Diagnose COPD
Spirometry
Spirometry is a lung function test that measures the amount of air you inhale and exhale. In spirometry, the patient takes a deep breath in and then exhales as hard and as long as possible into a hose connected to a machine called a spirometer. The machine measures how fast air is blown out of the lungs, as well as the total amount of air inhaled and exhaled (see Box 3-2, “What a Spirometer Measures,” on page 18). The results will be abnormal in someone with COPD.
Generally, after taking a spirometry test, the patient is given a bronchodilator medication to inhale. Then the test is repeated. If results improve after taking a bronchodilator, the patient likely has asthma rather than COPD, since asthma is often reversible. If COPD is present, airflow will continue to be limited, even after taking the drug.
Chest X-Ray
Some patients will be given a chest X-ray to see if the changes consistent with emphysema are present. A chest X-ray can also reveal whether the symptoms might be caused by a condition such as heart failure.
Computed Tomography

Computed tomography (CT) is another noninvasive imaging test that may be used to detect emphysema or bronchiectasis. It also may be used to decide whether a patient with COPD is a candidate for lung surgery.
Arterial Blood Gas Test
An arterial blood gas test may be performed to measure the amount of oxygen and carbon dioxide in the blood. It is used to determine whether there is too little oxygen in the blood (a condition called hypoxemia), or to detect the presence of too much carbon dioxide (called hypercapnia).
Blood Tests
In people younger than age 40 with the characteristic signs and symptoms of COPD, the physician will likely order a blood test to determine if the cause is a genetic condition known as alpha-1 antitrypsin deficiency (see Chapter 2). The test also may be ordered for someone with COPD symptoms who has a strong family history of COPD, or a family history of the enzyme deficiency.
The post 3. Diagnosing COPD appeared first on University Health News.
Read Original Article: 3. Diagnosing COPD »
Powered by WPeMatico