Skin Problems Are Common in Older Adults
Even if you never had skin problems in your youth, it’s common to suffer from rashes in your later years—as is underlined by a 2020 study (Journal of the American Geriatrics Society, November issue) suggesting that the majority of participants had at least one skin disease that required treatment or follow-up.
For the study, 552 people age 70 and older underwent a whole-body skin examination which revealed that nearly 76 percent of them had at least one skin disease that required treatment or followup and 39 percent had three or more skin diseases. Fungal skin infections were the most common, along with dermatitis and rosacea. Other common skin problems in older adults include psoriasis and pressure injuries. Here’s what you need to know about all of them.
Fungal Skin Infections
Fungal skin infections diagnosed in the study included tinea pedis (commonly referred to as athlete’s foot)—which affected nearly half the participants—and onychomycosis (a fungal infection of the nail bed), which was present in 30 percent of the participants. Another common fungal infection in older adults is candida albicans, a yeastlike fungus that is a particular problem for people with diabetes.
• Athletes foot causes redness, blisters, itching and peeling, particularly between the toes. You can treat the condition with over-the-counter (OTC) antifungal powders, sprays and creams, but symptoms can be difficult to eradicate. “If you don’t see an improvement within a couple of weeks, discuss with your doctor whether a prescription antifungal treatment may be needed,” says Annemarie Uliasz, MD, assistant clinical professor of dermatology at Mount Sinai. “Yeasts and fungi like warmth and moisture, so keeping your feet clean and dry can help prevent athlete’s foot. Change your socks often, and apply antifungal foot powder at each change.” Since athlete’s foot is contagious, avoid walking barefoot in gym locker rooms and when poolside.
• Onychomycosis begins as a white or yellow patch under one of the toenails (the fingernails also can be affected, but this is less usual), and progresses to cause discoloration, thickening, and crumbling of the nail. In severe cases, onychomycosis can be painful. “Fungal nail infections can be difficult to treat, and OTC products are not always effective,” says Dr. Uliasz. “If necessary your doctor will prescribe topical antifungal medication, but be prepared to use it for up to a year to see results. If the condition persists and is causing pain, or if you have diabetes, which increases the risk of more severe skin infections, your doctor may recommend an oral antifungal medication.”
Similar precautions as those recommended for preventing athlete’s foot can help you avoid onychomycosis. Also wash your hands after touching the affected nail, trim your nails straight across, and don’t wear nail polish and/or artificial nails. The former may reduce the effectiveness of antifungal treatments and the brush may spread the fungus to other nails, while the latter can trap moisture, which increases the risk of fungal nail infections.
• Candida albicans About one-third of people with diabetes suffer from skin itching and rashes due to circulation problems and the presence of candida albicans. Rashes may manifest as small red bumps, yellow or brownish patches, darker areas of skin that feel like velvet, blisters, and/ or open sores. If you have diabetes, the American Academy of Diabetes suggests using baby powder where skin touches skin (for example, between the toes and in skin folds). Opt for cornstarch-based powder, since there have been some safety concerns surrounding powders that contain talc. Avoid hot baths and showers, and when moisturizing after a bath or shower, avoid putting lotion between your toes.
Dermatitis
Dermatitis appears as an itchy, scaly rash that may ooze and become infected if scratched.
There are various different types of dermatitis. “In older adults, dermatitis tends to occur due to excessive dryness of the skin, in which case it is known as asteatotic dermatitis, or winter itch,” says Dr. Uliasz. “Atopic dermatitis—or eczema—commonly appears in people with a history of asthma or allergies, and often involves the creases of the elbows and knees. Contact dermatitis results from a reaction to an irritant or allergen, such as poison ivy, poison oak, or ingredients in cosmetics, skin lotions, fragrances, shampoos, and household cleaners.” Dr. Uliasz adds that neurologic diseases, such as Parkinson’s disease, predispose older adults to seborrheic dermatitis (commonly known as dandruff), which typically affects the scalp and face. People who are overweight, and those with poor circulation, high blood pressure, heart disease, kidney problems and/or a history of blood clots are particularly susceptible to stasis dermatitis, in which sore, itchy patches develop on the skin of the lower legs, typically in areas where varicose veins are prominent.
All types of dermatitis benefit from gentle skin care. “Use a bland, fragrancefree cleanser, and moisturize frequently with an emollient that contains ceramide,” Dr. Uliasz advises. Ceramide is particularly effective because it forms a barrier that helps prevent moisture loss from the skin. “Be sure to keep showers and baths brief and warm, rather than long and steaming hot,” Dr. Uliasz adds. Mild dermatitis also can be soothed with OTC hydrocortisone ointments. “More severe cases often require prescription corticosteroids, ultraviolet light therapy, or oral medications,” says Dr. Uliasz. “Seborrheic dermatitis may respond to OTC anti-dandruff shampoos or prescription-strength shampoos containing corticosteroids and/or antifungals.”
Applying cool, moist compresses also can ease soreness and itching due to dermatitis, as can an oatmeal bath. “Wear loose, breathable, cotton fabrics next to your skin, and trim your fingernails short to reduce any skin damage from scratching,” Dr. Uliasz says. “Wearing cotton gloves overnight is another good anti-scratching measure.”
Rosacea
At least 16 million Americans have rosacea, according to the National Rosacea Society, with women particularly vulnerable. The condition causes acnelike bumps, visible blood vessels, and excessive reddening of the skin on the cheeks, forehead, chin, and nose—other symptoms include burning, itching, or stinging; dry or thick skin; facial swelling; and eye irritation. “Rarely, rosacea may cause thickened skin on the nose that makes the nose appear bulbous,” Dr. Uliasz adds.
Rosacea may be triggered by hot drinks, spicy foods, temperature extremes, sunlight, and some drugs, including blood pressure medications. “Take care to avoid as many of these triggers as you can, stick to non-soap alcohol-free gentle facial cleansers, and protect your skin from the sun with a daily facial sunscreen that has a sun protection factor of 30 or greater,” Dr. Uliasz advises. “If rosacea is particularly bothersome, your doctor may prescribe topical treatments to reduce the redness and bumps. Laser treatment can effectively treat facial redness and visible blood vessels.”
Pressure Injuries
Older adults who are bedbound or have to sit for any length of time are susceptible to pressure injuries (also known as bedsores) on the skin in areas of the body that have less fat to pad them (for example, the heels, hips, base of the spine, and shoulder blades). Conditions that affect circulation—such as heart disease or diabetes—place you at greater risk of pressure injuries.
If you need bed rest following illness, surgery or injury, use pillows or supportive foam wedges as extra padding under the areas that are most vulnerable to pressure injuries, and place a pillow under your calves to raise your heels off the mattress. Change your resting position at least every hour (ask for help to do so if necessary), and ensure that the bed sheets remain smooth under your body. Also check (or ask a nurse or family member to check) for signs that a sore may be forming—for example, spots and reddish, darker-colored (or grayish if you’re Hispanic or African- American) areas of skin over bony areas, and patches of skin that itch or feel hot to the touch.
Psoriasis
Psoriasis is a chronic condition in which skin cells develop at an abnormally fast rate, rise to the surface of the skin, and accumulate. “This results in thick, inflamed skin with silvery scales, typically on the elbows, knees, legs, lower back, and scalp,” Dr. Uliasz explains.
Psoriasis can be triggered by infections, injuries to the skin (including sunburn), smoking, and certain medications, including beta-blockers, lithium, and antimalarial drugs. “Flare ups can be managed by applying topical corticosteroids,” Dr. Uliasz says. “Your doctor also may recommend products containing salicylic acid, which reduces the scaling associated with psoriasis, and coal tar, which helps ease itching and inflammation. For more widespread psoriasis, ultraviolet light therapy and biologic treatments that normalize the body’s overactive immune system are employed.”
Caring for Your Skin
Age-related changes make dry skin more likely as you get older, so take steps to ensure that your skin stays moist. Avoid excessively hot showers and/or baths, and use soaps that contain glycerin or other moisturizers. After a shower or bath, gently pat your skin until it’s barely dry, and then apply a lotion, body oil, or moisturizer that is high in ceramides or thicker emollients, like petroleum jelly. “Drink lots of fluids, and minimize your intake of caffeine and alcohol, since these can cause you to become dehydrated,” Dr. Uliasz advises. “Wash your clothes and bedding in detergents that are free of perfumes and fabric softeners that could irritate your skin. It’s also a good idea to schedule a yearly exam with a dermatologist who can advise you on any skin issues you may have.” And don’t forget skin cancer prevention measures—see our May issue for tips.
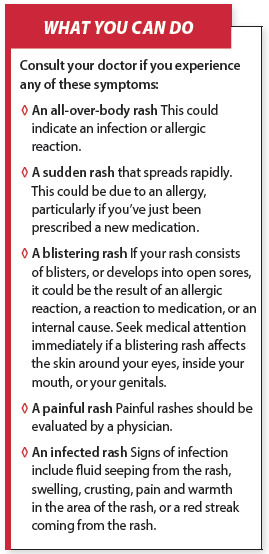
Keep in mind that itchy skin can signal a serious underlying problem, such as liver disease, kidney failure, thyroid disorders and some cancers. See What You Can Do for symptoms that warrant a visit to your doctor.
The post Skin Problems Are Common in Older Adults appeared first on University Health News.
Read Original Article: Skin Problems Are Common in Older Adults »