Minimize Plantar Fasciitis Pain and Protect Foot Mobility
Heel pain is one of the most pervasive foot complaints among older adults— not surprising since most Americans log about 75,000 miles on their feet by the time they reach age 50. A common cause of heel pain is plantar fasciitis, a condition characterized by pain in the morning when you take your first step, followed by slight improvement, and then an increase in pain later in the day. People who are particularly susceptible to plantar fasciitis are older women, people who are obese, and those who have a condition that degenerates and inflames the joints and tissues, such as arthritis. In the absence of proper care or treatment, plantar fasciitis may limit mobility, making it difficult to perform everyday activities, such as grocery shopping, walking, and exercising.
What Is Plantar Fasciitis?
As you step and your heel strikes the ground, a large amount of tension is placed on the fascia, which causes microtrauma— tiny tears in the tissue. The pain originates in the plantar fascia (PF), a band of tissue that extends lengthwise from your heel to the ball of your foot. If the tension on this tissue is too great, the fascia can develop small tears and become inflamed, which is what causes the pain. You are at greater risk of plantar fasciitis if you have a high arch, or are flat-footed or overweight. You’re also more likely to develop this condition if you rely on footwear that lacks adequate support, such as flat shoes or flip-flops.
First-Line Treatments
Consult a podiatrist. A consultation, as well as x-rays or other imaging, will help identify the origin of the pain and set the course for appropriate treatment.
Try nonsurgical treatment methods first. Remedies for plantar fasciitis typically start with nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen, which may reduce swelling and pain. Other options include rest, ice, physical therapy, orthotics, and steroid injections. More than 90 percent of patients with plantar fasciitis will improve within 10 months of starting non-surgical treatment methods.
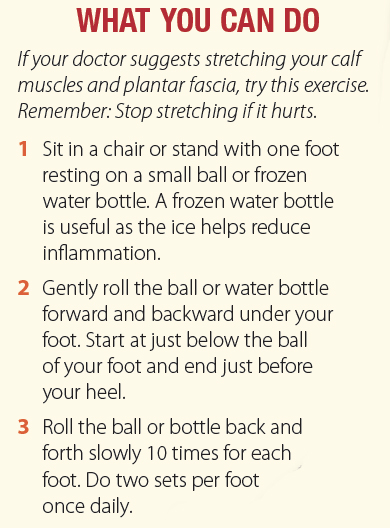
While stretching sometimes helps, there are instances when it can do more harm than good, depending on exactly what is causing the pain. “If it hurts when you stretch, stop stretching,” warns John J. Doolan, DPM, FAC-FAS, clinical assistant professor of podiatry in surgery at Weill Cornell Medicine.
Wear the right shoes. When plantar fasciitis is diagnosed, shoes with thick soles and extra cushioning can reduce pain that occurs with standing and walking. If you are experiencing heel pain, Dr. Doolan says, “Stop wearing flat shoes or going barefoot—even in the house.”
A cushioned shoe or insert reduces the tension and microtrauma that occurs with every step. To prevent or ease plantar fasciitis, choose shoes with good arch support and adequate cushioning, avoid going barefoot, and maintain a healthy weight. Soft silicone heel pads help by raising and cushioning your heel, and over-the-counter (OTC) or custom shoe inserts (orthotics) can also help cushion the foot and help it maintain an upright rather than tilted position. When considering an OTC orthotic, Dr. Doolan recommends, “Look for firm support and a heel that provides a one-quarterto one-half-inch lift.”
Next-Level Nonsurgical Treatments
If you still have symptoms after several months of rest, ice, and stretching, your doctor may recommend cortisone injections. Cortisone, a type of steroid, is a powerful anti-inflammatory medication that can be injected into the plantar fascia to reduce inflammation and pain.
“Cortisone injections are the standard of care and work very well, with little to no downtime, but there are many minimally invasive methods if injections fail,” says Dr. Doolan. Two of the newest nonsurgical plantar fasciitis treatment methods include extracorporeal shock wave therapy (ESWT) and ultrasound guided dry needling. ESWT applies high-frequency sound waves to the damaged PF to stimulate the body to repair itself. ESWT is especially effective for jump-starting the healing process in slow-to-heal connective tissues.
Ultrasound guided dry needling uses thin non-medicated needles—similar to acupuncture needles—to penetrate trigger points that contribute to PF pain. The needles evoke a twitch response in the muscle fibers that causes them to relax, providing immediate pain relief.
Prevent Further Foot Damage
If you feel pain in your heel as you take your first step in the morning, schedule an appointment with a podiatrist so you can get started on a plan of treatment to prevent further damage. Heel pain can be distressing and may even impede mobility, but Dr. Doolan maintains that conservative care, such as NSAIDs, orthotics, and stretching, often provides effective pain relief.
The post Minimize Plantar Fasciitis Pain and Protect Foot Mobility appeared first on University Health News.
Read Original Article: Minimize Plantar Fasciitis Pain and Protect Foot Mobility »

