Relieve Vaginal Dryness and Revive Your Postmenopausal Sex Life
Vaginal dryness due to declining estrogen levels is one of the most common complaints among postmenopausal women. “For many women, this means painful sex. My patients ask if there’s anything that can be done to restore their sex life, and my answer is almost always ‘yes,’” says Margaret Polaneczky, MD, a gynecologist at Weill Cornell Medicine.
Start With OTC Products
For most women, the first step is a trial of nonhormonal therapy. You’ll need two things: a moisturizer and a lubricant. “The menopausal vagina needs moisturizer, just like aging skin does. It doesn’t have to be every day, but it has to be regular and consistent, whether or not you’re having sex. One nonprescription, over-the counter (OTC) moisturizer, Replens, has been shown to be as effective as vaginal estrogen. Newer products containing hyaluronic acid seem to be effective as well,” says Dr. Polaneczky.
Vaginal Estrogen
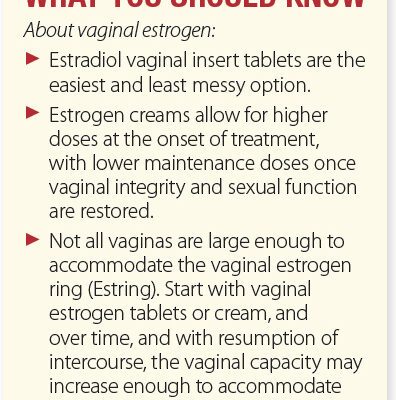
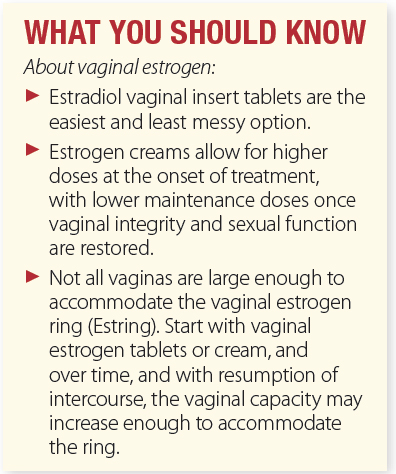
If moisturizers and lubricants aren’t enough, another possible fix is vaginal estrogen. Vaginal estrogen comes in three forms:
Estradiol tablets and inserts (Vagifem, Yuvafem, Imvexxy, and generics): These are placed into the vagina nightly for two weeks, then twice a week thereafter.
Estrogen creams (Estrace, its generics, and Premarin): The cream is inserted into the vagina nightly for two weeks, then two to three times a week thereafter.
Estradiol vaginal ring (Estring): This is a flexible ring that is inserted into the vagina every three months and continuously releases small doses of estrogen. The ring is a good option for women experiencing migraines from intermittent vaginal estrogen use. Dr. Polaneczky notes that not all vaginas are large enough to accommodate the ring. In that case, start with the vaginal estrogen tablets or cream. Over time, and with resumption of intercourse, the vaginal capacity may increase enough to accommodate the ring.
Estrogen Safety
Many women are concerned about potential health risks from vaginal estrogen; however, Dr. Polaneczky explains that estrogen exposure from vaginal estrogen is low, and blood levels of estrogen remain within the menopausal range. “In the large, prospective Women’s Health Initiative and Nurses’ Health studies, no increases in heart disease or cancers, including breast cancer, were noted among women using vaginal estrogen. That said, breast cancer survivors or women at high risk for breast cancer, especially those taking hormonal treatment to treat or prevent breast cancer, generally should avoid even the small amounts of hormone in vaginal estrogen,” says Dr Polaneczky.
Vaginal Dehydroepiandrosterone (DHEA)
DHEA, or Prasterone, is a suppository inserted daily in the vagina, where it is converted in the vaginal mucosa cells to estrogen and testosterone, which together mitigate vaginal dryness. Prasterone has been shown to be both safe and effective, with minimal impact on hormone levels throughout the rest of the body. “DHEA may be useful in women with estrogen-induced migraine or other sensitivity to vaginal estrogen products, or who are unresponsive to vaginal estrogen,” says Dr Polaneczky.
Other Alternatives
Ospemifine (Osphena) is the only oral FDA-approved medication for treating postmenopausal vaginal dryness, and is taken daily. Ospemifene is a selective estrogen receptor modulator (SERM), meaning that it acts like estrogen but contains no estrogen. Like estrogen, ospemifene carries a small risk of blood clots, but several studies have now shown no increase in clots among realworld ospemifene users.
While some small studies suggest lasers are effective therapy for vaginal dryness, laser therapy is currently not FDA-approved. It also is quite costly and not covered by insurance. “Until we have more and better research, I am not recommending laser treatments to my patients,” says Dr Polaneczky.
If postmenopausal dryness has persisted untreated for some time, the vagina may have decreased in size, making intercourse impossible. In this case, a course of vaginal hormonal treatment can be followed with use of vaginal dilators to gradually increase vaginal capacity.
Having vaginal dryness doesn’t mean your sex life is over. Have a frank discussion with your gynecologist if you need more guidance on the treatment options that are available. Dr. Polaneczky’s final recommendation: “Keep having sex. Sexual activity, including masturbation, increases blood flow to the vaginal tissues, which helps lubrication. The adage ‘Use it or lose it,’ really does apply here.”
The post Relieve Vaginal Dryness and Revive Your Postmenopausal Sex Life appeared first on University Health News.
Read Original Article: Relieve Vaginal Dryness and Revive Your Postmenopausal Sex Life »