OTC Pain Relievers May Pose More Risks Than You Realize
About 50 million U.S. adults suffer from chronic pain—having pain on most days for the past six months—according to statistics from the Centers for Disease Control and Prevention. Those 50 million people translate into about 20 percent of American adults, many of whom take over-the-counter (OTC) pain relievers.
But before you grab that bottle of of pills, keep in mind that OTC pain relievers come with possible harmful side effects just like prescription drugs do.
“People assume OTC products are safe to use as needed since no prescription is required, but most don’t understand the severity or the significance of the risks, especially with regular, long-term usage and/or high doses,” says Lisa Witkin, MD, pain management specialist and assistant professor of anesthesiology at Weill Cornell Medical College. “If someone is using high doses of OTC pain relievers for long periods of time, he or she needs to have a discussion with his or her doctor to consider other options.”
NSAID Warnings
The U.S. Food and Drug Administration (FDA) has warned that taking the nonsteroidal anti-inflammatory drugs (NSAIDs) ibuprofen (Advil, Motrin) and naproxen (Aleve) have been associated with an increased risk of cardiovascular diseases and events, including heart attack, stroke, and heart failure.
The FDA noted that the risks of heart attack and stroke increase even with short-term use, and the risks likely increase further with higher doses of NSAIDs taken for longer periods of time.
“Another risk of NSAIDs is that they can cause bleeding in the gastrointestinal (GI) tract. This risk is higher for patients who take blood thinners or who are at increased risk of GI bleeding for other reasons,” says Dr. Witkin.
You’re at higher risk for GI bleeding if you have a peptic ulcer or an H. pylori infection in your stomach. The “blood thinners” mentioned by Dr. Witkin include warfarin (Coumadin), apixaban (Eliquis), clopidogrel (Plavix), dabigatran (Pradaxa), rivaroxaban (Xarelto), and ticagrelor (Brilinta).
Possible consequences of GI bleeding include significant blood loss and a perforated ulcer. Sudden, severe bleeding can cause shock, which may result in unconsciousness. Symptoms of shock include a rapid pulse, minimal or no urination, and dizziness. In extremely severe cases, GI bleeding can cause death.
Aspirin Has Risks, Too
Aspirin is also an NSAID, although it does not carry the same dangers to heart health as ibuprofen and naproxen.
Often, a low-dose (81 milligrams) daily aspirin is recommended for people with cardiovascular disease who have had a heart attack or stroke, cardiac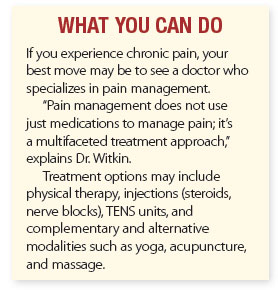 bypass surgery, or who have had stents placed in their coronary arteries.
bypass surgery, or who have had stents placed in their coronary arteries.
In 2019, a survey revealed that about 29 million Americans who did not have heart disease were taking low-dose aspirin, but the American College of Cardiology and the American Heart Association advised against this practice after research revealed that the benefit of taking a daily aspirin was offset by the risk of internal bleeding, especially for people ages 70 and older.
“Talk with your doctor to find out if the possible benefit of taking low-dose aspirin outweighs the risks for you. Not everyone should be on it for prophylactic [preventive] purposes,” advises Dr. Witkin.
Acetaminophen: Not an NSAID
Acetaminophen (Tylenol) relieves pain by a different mechanism than NSAIDS, and it is usually recommended as the first choice for people with cardiovascular disease. However, acetaminophen isn’t risk-free, either.
“Your body clears safe doses of acetaminophen, but high doses can cause liver damage,” says Dr. Witkin. “We worry about the cumulative dose patients may be getting without realizing it, since acetaminophen is included in hundreds of combination OTC and prescription medications.”
Experts now advise limiting acetaminophen to 3,000 milligrams a day, especially for people who weigh less than 150 pounds and/or take it frequently or daily.
“To avoid taking too much acetaminophen, check the labels of all OTC products, especially cold and flu medicines, to see if acetaminophen is listed as an active ingredient. If you have questions about what strength and dosage is right for you, talk to your doctor or pharmacist,” advises Dr. Witkin.
The take-home message: Choose your OTC pain reliever carefully, and always use the smallest amount for the shortest period of time possible.
The post OTC Pain Relievers May Pose More Risks Than You Realize appeared first on University Health News.
Read Original Article: OTC Pain Relievers May Pose More Risks Than You Realize »
