Understanding Heart Disease in Women

© Science Photo Library | Getty Images
Heart disease kills more women than all cancers combined.
Heart disease is the number one cause of death in both men and women. However, compared with men, women are more likely to die of a heart attack. Women also face a 20% increased risk of developing heart failure or dying within five years after their first severe heart attack compared with men, according to a 2020 research study published in the American Heart Association’s journal Circulation. In addition, women are less likely to be prescribed medications such as beta blockers or cholesterol-lowering drugs and have lower rates of revascularization procedures to restore blood flow, such as catheter-based angioplasty.
Why the Disparities?
Many of the poorer heart-health outcomes in women have to do with the fact that women have been underrepresented and historically excluded from heart disease clinical trials. The first National Heart, Lung, and Blood Institute (NHLBI) workshop examining heart disease in women took place in 1986. Women’s participation in heart trials have since increased, though there’s a long way to go to reach parity with men’s studies.
Studies direct the development of therapies and protocols, including evidence-based guidelines, diagnostic biomarkers and thresholds, risk factor identification, and medication recommendations. Much of today’s approach to heart disease prevention, diagnosis and treatment has been primarily based on the male heart. To be fair, it was once believed that men’s and women’s hearts were essentially the same. But as studies have rolled out, findings clearly show biological and functional differences between the sexes. These include:
The size and structure of the heart. A woman’s heart and blood vessels are smaller, and the muscular walls of women’s hearts are thinner.
Greater prevalance of coronary microvascular disease in women. This type of heart disease means the walls of the tiny arteries of the heart are damaged or diseased. The standard tests for coronary heart disease aren’t designed to detect coronary microvascular disease. The consequence of this is that women’s test results may incorrectly show that they’re at low risk for heart disease, and therefore they may not be offered preventive medications, such as statins and beta-blockers.
Differences in troponin. Troponin is a protein that can indicate that the heart muscle isn’t receiving enough oxygen because of an obstruction in its blood vessels. Physicians measure levels of troponin to help diagnose a heart attack. However, the blood levels of troponin that signal damage to the heart muscle in men is higher than in women. This means that tests may not be sensitive enough to detect the lower, but clinically relevant, level of troponin that would allow them to identify women’s heart attacks.
Evidence-based medicine relies on available data. When the evidence is lacking, diagnosis, treatment, and prevention for women may lag. Fortunately, knowledge gaps are closing. Programs such as the American Heart Association’s Go Red for Women (goredforwomen.org) tracks and posts some of the latest findings on women’s heart health.
How Menopause Affects the Heart
In premenopausal women, estrogen provides a protective effect on the heart. However, that changes after menopause. “In postmenopausal women, cardiovascular disease risk is increased,” says Marwah Shahid, MD, David Geffen School of Medicine at UCLA. “Several longitudinal studies show that there are distinct patterns of changes in sex hormones in women as we age and experience menopause. These hormone changes contribute to changes in body fat distribution, levels of cholesterol (lipids and lipoproteins) and the composition and structure of blood vessels.”
Some studies have suggested that hormone replacement treatments (HRT) for women may be beneficial for heart health; however, further research paints a different picture. “More recent robust clinical trials have not shown any cardiovascular benefit with hormone therapy on cardiovascular outcomes,” says Dr. Shahid. “There is also an additional risk for deep vein thrombosis and pulmonary embolism (blood clots in the legs and lungs, respectively) with the use of hormone therapy. We generally recommend an individual approach to the use of hormone therapy in women with significant vasomotor or genitourinary symptoms, with low- dose and short duration of hormone therapy use for patients with severe menopause symptoms. In patients with higher-risk disease including known heart disease, prior strokes, or breast cancer, we generally avoid hormone therapy.”

Understanding Risk Factors
Women over age 65 should pay particular attention to, and manage as needed, high blood pressure, obesity, and inflammatory and autoimmune diseases, as these put women at greater risk for heart disease. Though some of the risk factors for men and women are the same, studies have shown that these same factors raise women’s risk more. They include diabetes, having low levels of high-density lipoprotein cholesterol (HDL, a.k.a. good cholesterol), and smoking. The same lifestyle changes, however, can reduce risk in both sexes and include a healthy diet, such the Mediterranean diet or the DASH diet (Dietary Approaches to Stop Hypertension) and being physically active (at least 30 minutes of moderately vigorous aerobic activity five days per week).
“Several studies have shown that diet and exercise can significantly improve lipid profiles and reduce central obesity in postmenopausal women,” says Dr. Shahid. “The best time to start a heart healthy diet and exercise is now, since the effects of a long-term healthy lifestyle can help prevent and improve the pre-existing risk of cardiovascular disease-related outcomes.”
Heart Attack Symptoms in Women
Women with myocardial infarction (heart attack) can have angina (chest pressure and 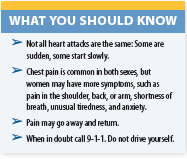 pain) just like men, but women are likely to have more symptoms, such as pain in the shoulder, back, or arm, and anxiety. According to the NHLBI, in women:
pain) just like men, but women are likely to have more symptoms, such as pain in the shoulder, back, or arm, and anxiety. According to the NHLBI, in women:
- Different activities bring on chest pain. In men, angina (chest pain/discomfort) tends to worsen with physical activity and go away with rest. Women are more likely than men to have angina while they are resting. In women who have coronary microvascular disease, angina often happens during routine daily activities, such as shopping or cooking, rather than during exercise. Microvascular angina events may last longer and be more painful than other types of angina.
- Mental stress. It is more likely to trigger angina pain in women than in men.
- The location and type of pain may differ. Pain symptoms are different for each person. Women having angina or a heart attack often describe their chest pain as crushing, or they say it feels like pressure, squeezing, or tightness. Women also may have pain in the chest or the neck and throat.
- Other symptoms common for women include nausea, vomiting, shortness of breath, abdominal pain, sleep problems, tiredness, and lack of energy.
According to the American Heart Association, heart attacks can be sudden and intense, but most start slowly, with mild pain or discomfort that gradually worsens over a few minutes. These episodes might come and go several times before the actual heart attack occurs. If a symptom occurs out of the ordinary, during an activity or a stressful event, and doesn’t go away after you stopped the activity or at rest, seek emergency care by calling 9-1-1. Early treatment can limit damage to your heart, reduce the risk of heart failure, and can save your life.
The post Understanding Heart Disease in Women appeared first on University Health News.
Read Original Article: Understanding Heart Disease in Women »

