4. Skin Conditions: From Acne to Lupus
There are hundreds of noncancerous skin growths and conditions, and this chapter describes, in alphabetical order, 18 of the most common problems. An additional 18 are covered in Chapter 5. Most do not require medical attention, those that do are often unreported, but all of them should be monitored in case changes occur.
The exact cause of many noncancerous skin conditions is unknown (rosacea, for example), but scientists have discovered the origins of several familiar abnormalities.
Warts are caused by viruses, athlete’s foot by a fungal infection, and boils by bacteria. Rashes can be triggered by allergens, Lupus is an autoimmune disease, and seborrheic keratosis has a genetic link. Stress and environmental irritants can trigger or make skin problems worse.
Cold sores, measles, and poison ivy are contagious, but psoriasis, hives, and eczema are not.
At-home treatment is often possible with over-the-counter or prescription medications. When medical procedures are required to remove a growth, it can be done with an electric needle, a scalpel, a laser, or by freezing with liquid nitrogen. Almost all procedures can be performed in the office of a dermatologist.
The take-away message is that being knowledgeable about skin growths, conditions, and abnormalities—noncancerous in this chapter and in the following chapters—enables you to make informed decisions about your own skin health and that of your family.
Acne: Not Just for Teens
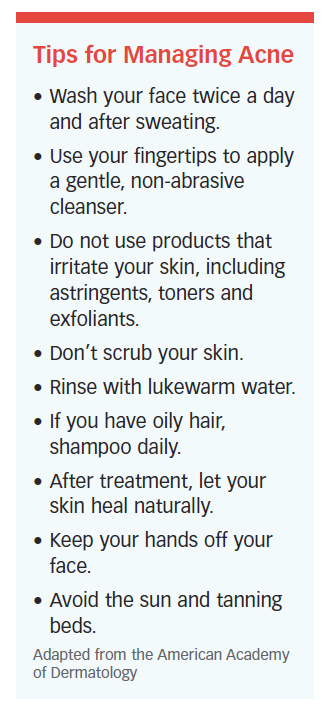
The most common skin condition in the U.S. is acne, which affects as many as 50 million people annually, and it’s not limited to teenagers.
According to American Academy of Dermatology (AAD), most cases of acne are seen in teenagers, but adult men and  women can also get the condition (even in middle age).
women can also get the condition (even in middle age).
Acne is inflammatory, chronic, and develops when hair follicles get plugged with oil. It can be affected by stress, humid climates, oil-based makeup, and hormonal changes.
Dermatologists may grade acne on a 1-4 scale—1 is mild, 4 is severe—but there is no universally accepted grading system. Once diagnosed, mild cases can be controlled with over-the-counter topical medications that either kill the bacteria or reduce the production of oil. The medicine may contain a retinoid, benzoyl peroxide, antibiotic, or salicylic acid. Isotretinoin, says the AAD, is the only treatment that is effective in all cases of acne.
More serious cases are treated with lasers, other light therapies, chemical peels, or a “drainage and extraction” procedure to remove a large cyst.
Treatment is individual in nature. What works for one person may not work for another. Without treatment, acne can cause permanent scars. Treatment should continue even when the skin clears.
Athlete’s Foot
 Athlete’s foot is an infection caused by a fungus, according to the American College of Foot and Ankle Surgeons. It develops because feet spend a lot of time in the perfect breeding environment of warm, dark, humid shoes.
Athlete’s foot is an infection caused by a fungus, according to the American College of Foot and Ankle Surgeons. It develops because feet spend a lot of time in the perfect breeding environment of warm, dark, humid shoes.
The symptoms are redness, small blisters, itching, and peeling, especially between the toes. Once the infection develops, it can be challenging to cure. It’s rare, but the infection can spread to other parts of the body, including the toenails. Treatment options include over-the-counter antifungal powders, sprays, and creams, and prescription antibiotic medications. If things don’t get better within two weeks, see your doctor.
Prevent symptoms by keeping your feet clean and dry. Wear wicking acrylic or cotton socks. It’s the same infection that causes Jock itch, so men should wear socks before putting on underwear. Change shoes, socks, or stockings often, and use foot powder daily. Avoid walking barefoot, especially in humid public places, such as locker rooms.
Blisters
Blisters are small pockets filled with fluid that develop on the upper layer of skin, which is trying to protect itself. They are usually caused by friction.
Treatment starts with covering the blister with a bandage. If the blister is in an area of the foot that can be protected, use padding to protect it. Cut the padding into a donut 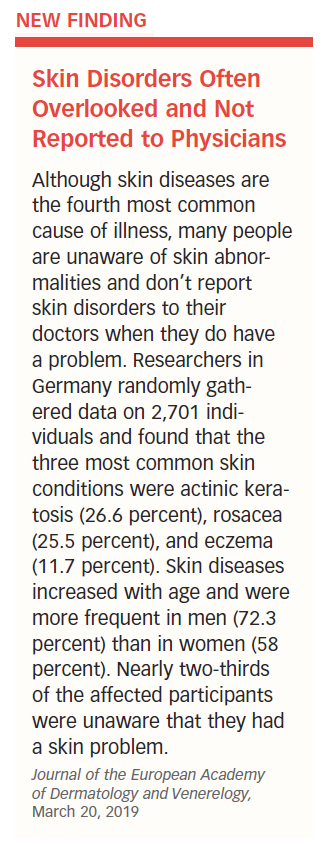 shape with a hole in the middle, then place it around the blister. Cover the padding with a bandage. Avoid popping or draining a blister if possible, as it could lead to infection.
shape with a hole in the middle, then place it around the blister. Cover the padding with a bandage. Avoid popping or draining a blister if possible, as it could lead to infection.
If a blister is large and painful, sterilize a small needle with rubbing alcohol, pierce the edge of the blister and allow some of the fluid to drain. Do not remove the skin.
Here are some tips from the AAD for protecting your feet from blisters:
- Wear nylon or moisture-wicking socks.
- Try wearing two pairs of socks.
- Make sure your shoes fit properly—not too tight or too loose.
- Use powder or petroleum jelly to reduce friction when your skin rubs together or against shoes.
- Stop an activity immediately if you experience pain or discomfort, or your skin suddenly turns bright red.
Boils
A boil is a skin infection that develops around a hair follicle. Common sites are the face, neck, armpits, buttocks, groin, and thighs. Boils begin as a red, elevated, warm, and painful bump on the skin, which is often caused by an infected hair follicle. A foreign object (like a splinter) embedded in the skin, a plugged sweat gland, or blocked oil duct also can trigger boils.
A staphylococcus infection is often the main culprit. Individuals with diabetes, immune deficiencies, poor nutrition, and poor hygiene are at a greater risk for boils than the general population.
As boils grow, the area may get bigger, softer, and even more painful. Within a week, the area turns white as pus makes its way to the surface. Sometimes it drains through the skin. At other times, it has to be lanced and drained by a physician. Several boils can develop at the same time because the infection spreads to the surrounding area, or is transported to some other part of the body.
Warm Compresses to Ease Pain
Warm compresses or soaking the boil in warm water for 20 minutes, three or four times a day can ease the pain. The increase in temperature draws the pus closer to the skin’s surface and allows it to eventually drain out.
increase in temperature draws the pus closer to the skin’s surface and allows it to eventually drain out.
Applying antibiotic creams on the area before the boil comes to a head will not work, because the medication does not penetrate the skin. “Coming to a head” means the top of the area breaks and the pus drains out, but the process could take as long as 10 days.
Lancing Could Spread Infection
Do not lance the boil yourself, as doing so could allow the infection to spread. If and when the boil does break, keep the area clean by gently washing it with an antibacterial soap two or three times a day. Apply a medicated ointment and cover the area with a bandage.
See a doctor if the infected area gets worse, if you develop a fever, if the boil does not drain, if additional boils appear, if the boil limits your normal activities, or if you have diabetes. Do not take chances. If in doubt, call your family doctor or a dermatologist.
Calluses/Corns
 Both corns and calluses involve a thick outer layer of skin, and both can be caused by pressure or toes rubbing together. They may also result from foot deformities or misshapen toes associated with rheumatoid arthritis.
Both corns and calluses involve a thick outer layer of skin, and both can be caused by pressure or toes rubbing together. They may also result from foot deformities or misshapen toes associated with rheumatoid arthritis.
The difference is that corns (and there are five types of them) have a core and normally develop on a knobby part of a toe, while calluses are evenly distributed on the soles of the feet. Although some calluses may protect a part of the foot, both corns and calluses can be big enough to cause pain and difficulty in walking.
Treat Only if Painful
When calluses and corns are painful, the goal of treatment is to reduce or eliminate the pressure or friction that causes them. Wear shoes that fit properly, use pads that cushion the area, and use an over-the-counter product (salicylic acid) that softens the tissue, making it possible to remove the dead skin. If you have diabetes, peripheral artery disease, or peripheral neuropathy, get medical attention.
Otherwise, neither corns nor calluses need treatment unless they cause pain. If possible, avoid the contact that causes the friction. If hands are affected, wear protective gloves. You can also relieve the pressure by using a doughnut-shaped pad on the foot. In rare cases, surgery is needed to remove a corn or callus.
You should not cut a callus or corn, especially if you have diabetes or any other condition that affects circulation, but you can gradually wear down the area with a pumice stone.
Prevention
Prevention is always better than treatment. Steps you can take to reduce your risk include not wearing tight, high-heeled, or loose-fitting shoes, or socks that do not fit. Walking barefoot can also cause calluses and should be avoided when doing so is the cause. See “Tips for Managing Corns and Calluses” for AAD suggestions.
Cellulitis
Cellulitis is a skin infection, most commonly caused by streptococcal bacteria. Symptoms include pain, warmth, redness and tenderness. It is caused or associated with an injury to the skin that results in a small break, allowing the bacteria to enter. The majority of cases involve just one side of the body, most likely on the lower legs. It can also affect the skin around the eyes. In severe cases, the symptoms might include fever or chills, nausea, increased pain, headache, rapid heart rate, and low blood pressure.
At higher risk for cellulitis are those who have sustained an injury, have other skin conditions (such as eczema, athlete’s foot, or shingles), are obese, or have a weakened immune system.
Treatment with antibiotics usually resolves the problem within two or three days, but the symptoms may get temporarily worse before they subside. Rest, elevation, and over-the-counter pain relievers can help ease the discomfort. If an abscess develops, it has to be drained.
Washing wounds daily with soap and water, applying a protective cream or ointment, covering wounds with bandages, and watching for signs of increased infection are sound prevention methods.
Cold Sores
Cold sores (fever blisters) are caused by the herpes simplex virus (HSV-1), the oral form of the virus that never leaves the body once it has been contracted.
HSV-1 infects more than half of all people in the United States between the ages of 14 and 49, and up to 67 percent of people in the world. It is one of the world’s most contagious conditions, easily transmitted as a result of close contact.
The symptoms include fluid-filled blisters on the mouth that eventually break and ooze, sore throat, swollen glands, fever, and headaches. Outbreaks can occur in some people several times in one year.
The news is not all bad. Some fortunate people infected with the same virus never have an episode. It remains dormant throughout life. For those who experience cold sores, the condition is self-limiting—the unsightly symptoms run their course within two weeks.
Over-the-counter creams that contain acyclovir or penciclovir can shorten the duration of an episode. Prescription antiviral medications like acyclovir (Zovirax), famciclovir (Famvir), and valacyclovir (Valtrex) are effective for more serious cases. Reduce the chance of infecting others by:
- Not kissing people when symptomatic
- Avoiding close contact with those who have a weakened immune system
- Not sharing personal items that come into contact with the face
- Not sharing food or drinks
- Not touching a cold sore
- Washing your hands frequently
Cysts
Sebaceous, keratin, epithelial, and epidermoid are terms used to describe small, fairly common cysts that develop just below the surface of the skin. The U.S. National Library of Medicine refers to them as epidermoid cysts.
Epidermal cysts are sacs beneath the skin’s surface filled with keratin and fatty material. They often develop at the site of a damaged hair follicle on the face, neck, trunk, genital area, and behind the ears. In some cases, there is an opening in the center through which the foul-smelling fatty content of the cyst can escape.
Cysts can move around (under the skin) within a small area. They can become tender, inflamed, and perhaps larger than when you first noticed them. Typical epidermal cysts range in size from one-quarter inch to two inches. When inflammation is involved, cysts are likely to be tender and red, and the temperature of the skin on top of the growth may rise.
Risk factors for cysts are age (most people get them during their 30s or 40s), gender (men are twice as likely to get them as women), a history of acne, an injury to the skin (any type of crushing or traumatic injury), and long-term sun exposure.
Most Require No Treatment
Epidermal cysts are not dangerous, and most require no treatment. If you think one has become inflamed, or if you have one that is large or painful enough to interfere with daily activities, your doctor can diagnose the condition with an examination. In some cases, a biopsy can rule out more serious skin conditions.
A warm compress might help drain the cyst—do not force the drainage—or your doctor might inject the area with a steroid to reduce inflammation. On rare occasions, surgery is required to remove it. Cysts may recur. You cannot prevent these growths, but avoiding excessive sun exposure and using skin products that do not contain oils might help.
Dermatitis
Coming into contact with foreign substances triggers most rashes and skin irritations. The one that is most likely to cause problems in older adults is dermatitis. The two most common forms are allergic contact dermatitis and irritant contact dermatitis.
A third form is called atopic dermatitis (atopic eczema), a condition passed from parents to children that can develop at any time during a person’s life. It is primarily a problem for infants and children.
Eczema
Eczema is not one condition, it’s at least seven. In one form or another, eczema affects more than 30 percent of the U.S. population.
Up to 18 million Americans have symptoms of eczema. Ninety percent of those who get the form known as atopic dermatitis (AD) do so before the age of five, and half of them continue to have symptoms for a lifetime. It’s manageable but not curable. The condition is not contagious, but it runs in families. The symptoms are different in adults than they are in children. Its cause is a mystery. The AD variety of eczema comes with lots of baggage. Knowing what to look for and what to do about it won’t cure the skin disorder, but it can make living with AD less painful and less stressful.
Symptoms (in adults):
- Dry, scaly skin
- Itchy skin
- Thickened or cracked skin
- Rash that is red, swollen, and sore
- Rash that gets worse with scratching
- Rash or bumps that may leak clear fluid
- Rash that becomes infected
The most common places for the rash to appear are the cheeks, wrists, hands, behind the knees, in the creases of elbows, and on the buttocks. For those who have had AD flares (flare-ups) in childhood, their experience of symptoms tends to be much milder in adulthood.
Contributing Factors of AD. The exact cause of AD is unknown, but there are plenty of contributing factors. You are more likely to have AD if a family member has it—or allergies, or hay fever, or asthma. The connection has to do with a genetic variation that alters the skin’s ability to protect itself. The crossed signals also cause the body to overreact to outside forces—triggers—including:
- Scratchy clothes
- Cleaning products
- Soaps
- Dust
- Animal dander and saliva
- Excessive heat or cold
- Perspiration
- Stress
Foods (nuts, dairy products, eggs, fruit juices, soy products, wheat) do not cause AD, according to the AAD, but food allergies may make it worse.
The list of triggers is long, but not every person’s body responds to every one. Part of prevention is knowing which substances or events cause your particular symptoms and avoiding them. Diagnosis by a family doctor or dermatologist is relatively straightforward. It consists of taking a person’s medical history, observation of symptoms, and may require a blood or patch test to determine the trigger.
Treatment of Choice. Corticosteroids are the treatment of choice, but the U.S. Food and Drug Administration (FDA) has approved newer and effective gels, foams, and oils. In March 2017, the FDA approved dupilumab (Duprixent) in injection form to treat adults with moderate-to-severe AD. The medication is intended for patients whose eczema is not controlled by topical drugs or for whom topical therapies are not advisable. If AD is accompanied by a skin infection, antibiotic, antiviral, and antifungal drugs may be recommended. Antihistamines can produce drowsiness when taken at bedtime to reduce itching and scratching. Light therapy (phototherapy) uses ultraviolet (UV) rays to treat moderate cases of dermatitis.
Prevention. Among the home measures you can take is to apply an over-the-counter moisturizer/body lotion every day and within three minutes of bathing or showering, to capture moisture.
Here are other preventive measures:
- Take lukewarm baths (hot water can trigger a flare).
- Wear soft fabrics, not scratchy ones.
- Use mild or non-soap products.
- Use a humdifier when the weather is dry or cold.
Allergic Contact Dermatitis
This rash appears when the immune system overreacts to allergens like poison ivy, poison oak, poison sumac, cosmetics, latex, nickel, and hair dyes. Even the fragrances in certain soaps, shampoos, and perfumes can cause a reaction.
Antibodies from your immune system come into contact with the allergens and set off “mediators,” such as histamine, which cause the symptoms. Allergic contact dermatitis may appear almost immediately or a day or two after exposure. Symptoms include reddish skin or a rash, an itching or burning sensation, swelling, and blisters that ooze, break, and leave crusts or scales.
Drugs may cause problems themselves. Neomycin, a commonly sold over-the-counter topical antibiotic, and formaldehyde (a chemical found in building materials and some household products) are two examples that cause allergic contact dermatitis.
The American Contact Dermatitis Society selected isobornyl acrylate as the 2019 Contact Allergen of the Year. It is an acrylic molecule used as an adhesive. Among other applications, isobornyl acrylate is often used in medical devices. The selection was made based on multiple case reports of diabetes patients developing contact allergies to their diabetes devices, such as insulin pumps. Routine testing does not identify the substance, so it is very important that the clinician be aware of its danger.
Other Contact Allergens of the Year over this decade include:
- 2010: Neomycin (found in antibacterial products, tooth paste, creams, eye drops, pet food, deodorants, soaps, cosmetics, vaccines)
- 2011: Dimethyl fumarate (medications for multiple sclerosis, psoriasis, other medications)
- 2012: Acrylate (synthetic flavoring, fragrances, latex paints, dirt-release agents, paper coatings, floor polishes, sealants, shoe polishes, adhesives, acrylic nails, hearing aids, dental fillings)
- 2013: Methylisothiazolinone (laundry detergents, cream cleansers, window cleaners, countertop sprays, room sprays, stain removers, carpet shampoos, air fresheners)
- 2014: Benzophenones (nail polish, lip balm, sunscreen, soap, makeup products)
- 2015: Formaldehyde (mattresses, sheets, furniture, air fresheners, clothing)
- 2016: Cobalt (glass, pottery, crayons, costume jewelry, zippers, buckles, utensils, tools, dental plates)
- 2017: Alkyl glucoside (shampoos, skin cleansers, wipes, sunscreens, deodorants, moisturizers, shower gels, fragrances)
- 2018: Propylene glycol (soft drinks, frozen meals, spices, cake mixes, salad mixes, soups, soft drinks, artificial sweeteners)
- 2019: Isobornyl acrylate (adhesives, medical devices, nail polish)
Irritant Contact Dermatitis
This form of dermatitis is caused by a foreign substance that comes into direct contact with your skin and damages the area. Detergents and solvents are examples. They can wear down the skin’s protective surface. The longer the substance stays on the skin, the more serious the damage, and it could take up to four weeks for the area to return to normal. Symptoms and signs include pain, redness, scales, and even cracks in the skin.
Treatment. Treat itching and other symptoms of most rashes at home with cortisone-based creams to reduce inflammation. Other options are calamine lotions, oral antihistamines, and oatmeal baths. Over-the-counter drugs like Benadryl and Ben-Allergin may also help. Try to resist scratching, which will further inflame the rash.
For irritant contact dermatitis, wash the area with soap and cool water immediately after contact to get rid of the foreign substance. Treat any blisters that may form with cold, moist compresses 30 minutes at a time, three times a day. Seek medical help if the rash does not improve within two or three days, or if it continues to spread.
Diabetes and Skin
 Sometimes a skin disorder is the first sign that diabetes is present. Diabetes and skin issues are directly linked. The warm, high-sugar content of the blood is a perfect environment for the growth and development of skin-related bacterial and fungal infections. Anyone can get these skin conditions, but people with diabetes are more susceptible.
Sometimes a skin disorder is the first sign that diabetes is present. Diabetes and skin issues are directly linked. The warm, high-sugar content of the blood is a perfect environment for the growth and development of skin-related bacterial and fungal infections. Anyone can get these skin conditions, but people with diabetes are more susceptible.
A common symptom of many diabetes-related skin diseases is itching. It can be caused by a variety of issues, including dry skin, yeast infections, or diminished blood flow to an area of the skin. Lower legs are affected more often than other regions of the body. Lotions and moisturizers can limit itching by keeping the skin soft and moist, but excessive amounts applied to certain areas create an environment conducive to infections.
The AAD has identified several skin-related problems associated with diabetes (see “12 Skin-Related Warning Signs of Diabetes”).
“If you have diabetes, try to avoid trauma and follow up with a podiatrist if your feet are involved or with a dermatologist for any skin conditions,” says UCLA’s Dr. Lorraine Young. (medical editor of this report).
Bacterial Infections
 Styes, boils, carbuncles (a cluster of boils), and nail infections are examples of bacterial infections that can occur in people with diabetes. The symptoms are hot, swollen, red, and painful spots, depending on the condition (styes on the eyelids; boils around hair follicles; carbuncles deep in the skin; nail infections on hands or feet). The most common type of bacterial infection is staphylococcus, or “staph,” for short.
Styes, boils, carbuncles (a cluster of boils), and nail infections are examples of bacterial infections that can occur in people with diabetes. The symptoms are hot, swollen, red, and painful spots, depending on the condition (styes on the eyelids; boils around hair follicles; carbuncles deep in the skin; nail infections on hands or feet). The most common type of bacterial infection is staphylococcus, or “staph,” for short.
Bacterial infections are treatable with antibiotics and perhaps preventable by controlling blood sugar levels. Nevertheless, people with diabetes are affected more than those without the disease. Only a doctor can diagnose the infection and prescribe medications, either in pill or cream form.
Fungal Infections
Athlete’s foot, jock itch, ringworm, and some vaginal infections are fungal infections that affect the general population, but which present special problems for people with diabetes. The cause is often a yeast-like fungus. It causes an itchy, red area surrounded by small blisters and scales, usually in warm, moist folds of the skin, such as the mouth, vagina, breasts, fingers, toes, nails, and rectum. The fungus can move through the bloodstream and affect other areas of the body, too.
Diabetic Dermopathy
This condition is caused by changes in small blood vessels that result in light brown, scaly, oval, or circular patches of skin, often on the front of the legs. The patches do not itch, hurt, or drain and usually do not require treatment.
Necrobiosis Lipoidica (NL)
This rare condition is caused by a change in the blood vessels, and consists of oval plaques, usually on the lower legs. It is similar to diabetic dermopathy, but the spots are larger, deeper, and fewer in number. NL may begin as small red or raised spots, which develop a shiny appearance surrounded by a violet-colored border. The spots often turn brown and fade, but often leave a permanent discoloration. NL can be painful and itchy. Adult women are more susceptible, and people with diabetes account for two-thirds of all cases. If the plaques break open, see a dermatologist for treatment.
Diabetic Blisters
People rarely develop diabetic blisters on their fingers, hands, toes, feet, legs, or forearms, but it can happen. They resemble blisters caused by burns, but are not painful. Diabetic blisters heal in two to three weeks without treatment. Those who develop the blisters often have diabetic neuropathy, a nerve disorder. The only way to guard against the incidence of diabetic blisters is to control blood sugar.
Eruptive Xanthomas (EX)
This condition develops when diabetes has gotten out of control. The symptoms are small, firm, yellow-red bumps on the skin. A red circle surrounds the bumps, and the area may itch. EX often appear on the backs of hands, feet, arms, legs, and buttocks. A person at risk has type 1 or type 2 diabetes and elevated blood lipids. However, the bumps disappear once the person’s blood sugar level returns to acceptable levels.
Prevention
The AAD suggests these measures to prevent or reduce the risk of diabetes-related skin diseases:
- Keep skin clean and dry by using cornstarch-based or talcum powder where skin touches skin.
- Avoid hot baths and showers, and do not put lotion between your toes. Warm, moist surfaces are breeding grounds for infections.
- Prevent dry skin by using moisturizers, especially in cold, windy weather.
- Treat cuts immediately. Wash them with soap and water, but avoid products that are too harsh, such as alcohol and iodine.
- Use antibiotic cream only if advised to do so by your doctor.
- Keep your home more humid than normal during cold, dry months.
- Bathe less, if practical.
- Use mild shampoos, and avoid feminine hygiene sprays.
Folliculitis
Folliculitis is a common skin condition in which hair follicles become inflamed. Follicles damaged by friction, blockage, or shaving can become infected with the staphylococcus (staph) bacteria. Folliculitis is easy to treat, but it may recur and the infection can spread to other areas of the body. Symptoms include a rash, itching, or pimples on the neck, groin, or genital area. Your doctor may be able to diagnose folliculitis with a visual exam. Lab tests show the type of disease agent that has caused the infection. Hot, wet compresses can help drain the area, and treatment may include oral or topical antibiotics. If self-care does not relieve symptoms within two or three days, contact a medical professional.
Granulomas
Granulomas are small nodules (bumps) that can develop all over the body and can range in severity from benign to malignant. They are relatively common in adults.
The two types that can affect the skin are called pyogenic granuloma (caused by an injury to the skin) and granuloma annulare (the most common form).
The pyogenic variety, most often found on the arms, hands, and face, might resolve without treatment, but most of the time they have to be removed surgically.
Granuloma annulare is more common in children and young adults. It may or may not disappear on its own, but can be treated with steroid creams or injections. In some cases, treatment involves a combination of medication followed by exposure to UV light.
Hives
This condition is produced by blood plasma leaking through small gaps between the cells lining the small blood vessels in the skin. The condition appears as red, raised areas in irregularly shaped sizes ranging from small to several inches across.
These welts, which have a red border, can develop anywhere on the body, including the arms, legs, and trunk, either alone or in groups. When the condition lasts longer than six weeks, it is classified as chronic hives. In both cases, flare-ups come and go, only to appear somewhere else on the body.
The person most likely to suffer from hives has had a previous episode, tends to have allergic reactions in addition to those resulting in hives, has a family history of hives, or has a non-skin-related disorder such as lupus, lymphoma, or thyroid disease.
Acute Reactions
Acute hives can last from a few hours to several weeks. It is often caused by the body’s reaction to certain foods (eggs, tomatoes, chocolate, nuts, milk, and shellfish, for example), medications (aspirin, penicillin, sulfa drugs, sedatives, antacids, laxatives, codeine, and others), stings (bees, wasps), or infections (hepatitis, strep throat, mononucleosis, colds). Physical factors, such as heat, cold, sunlight, water, pressure on the skin, exercise, and emotional stress, can also trigger episodes in 20 percent of cases.
Chronic Reactions
Not only do chronic hives last longer, but their cause is harder to detect. There is no specific test to identify the condition. In more than 80 percent of chronic cases, the cause is unknown, despite reviews of a patient’s medical history, physical examinations, blood work, skin tests, and biopsies. In about one-half of those cases, the body’s immune system triggers the release of histamines, which cause the fluid to leak from blood vessels and produce swelling.
In a related condition called angioedema, the swelling occurs underneath the skin rather than on top. Affected areas include the lips, eyes, hands, feet, and sometimes the genitals. The swelling caused by angioedema also may affect the throat, tongue, or lungs, and make breathing difficult. This life-threatening situation requires immediate medical attention.
Relieve the Symptoms
The goal is to relieve the symptoms, and that may be done with cool compresses or showers, damp cloths, loose-fitting clothes, minimizing vigorous physical activity, and avoiding uncomfortably warm environments.
Over-the-counter antihistamines like Allegra, Benadryl, Chlor-Trimeton, Claritin, Tavist, Xyal and Zyrtec offset the effects of the histamine produced by the body, as can prescription drugs, such as hydroxyzine (Atarax, Vistaril), and desloratadine (Clarinex). These medications may be taken in combination with drugs known as histamine-2 (H2) blockers, like Zantac and Tagamet.
The corticosteroid prednisone (Deltasone, Rayos, Sterapred), when taken orally, might control hives, but it is seldom recommended because of its side effects, such as fluid retention, increased blood pressure, and elevated pressure in the eyes.
Before taking any over-the-counter or prescription medications, let your doctor know which other drugs you take, including supplements. Doing so could prevent drug interactions and complications. Any type of drug therapy should be designed for your specific needs.
Avoid the Problem
Avoiding the substances and environments that causes hives is the best way to prevent them, but it is not always that easy. If you think foods are the problem, keep a log to detect suspect items or ingredients. Foods that can be associated with hives include:
- Eggs
- Milk
- Nuts
- Fish
- Berries
- Chocolate
- Tomatoes
Heat Rash
Heat rash is a hot weather-related condition that affects all ages. The condition is also known as prickly heat, miliaria, and summer rash. Regardless of what it’s called, the condition is an inflammation of the skin caused by blocked sweat glands. It is uncomfortable and itchy, but can be treated at home and usually goes away within a few days, with or without treatment.
Aging, Overweight, Humidity
Heat rash can affect just about anyone of any age. Those at highest risk are people who live in hot and humid climates, older adults, overweight individuals, exercisers, those who sweat a lot, and babies. It is often associated with babies because their sweat glands are not fully developed.
Blocked Sweat Glands
Sweat glands are located in the second layer of skin (the dermis). When sweat ducts are blocked, perspiration cannot get to the surface and evaporate. Instead, it gets trapped under the skin, where it causes mild inflammation resulting in a rash. The combination of sweating heavily when exercising while wearing clothes that don’t allow the sweat to evaporate can also trigger the rash. Heat rash can even happen during the winter if people wear too much clothing or sit close enough to a fire or heater to sweat.
Symptoms Indicate Type
Four types of heat rash have medical terms most of us wouldn’t recognize or use. They are easier to remember by how the rash looks—red, white, clear, or deep.
- Red heat rash is the most common form. It’s called “prickly heat” because it itches and burns.
- A yellow or white rash might be a sign of infection and is a reason to have it checked by a doctor.
- Clear heat rash looks like small, clear beads of sweat on top of the skin. It is the mildest form and is not likely to cause any discomfort or itching.
- Deep heat rash is caused by repeated episodes and chronically inflamed sweat glands. Deeper layers of the skin are affected and the rash may appear as large, firm bumps.
The most common places for the rash to develop are creases in the skin, such as the armpits, neck, and groin, where skin rubs against adjacent skin. Wearing tight clothes can prevent sweat from evaporating, especially around the waist, chest, or groin. Bandages and heavy creams or lotions can also block sweat glands.
Treatment and Prevention
Heat rash is uncomfortable but treatable. The first step is to stay cool. The rash may disappear simply by cooling the skin. If that doesn’t work, here are a few other suggestions:
- Avoid activities that cause sweating.
- Stay in the shade when outdoors and in air-conditioned spaces when inside.
- Wear loose-fitting, loose-woven, thin, moisture-wicking, quick-drying clothes.
- Take cool showers.
- Use mild, antibacterial soaps.
- Use over-the-counter, anti-itch medications that contain calamine, menthol, or camphor.
- Be careful about using oil-based skin products that can clog pores.
When to Call Your Doctor
Although heat rash can be uncomfortable, it is usually mild and goes away quickly. Common sense and home remedies are enough to keep the doctor away in most cases.
But if the rash doesn’t go away in a few days, see your doctor. If the area is painful, red, swollen, or warm, or if the lesions are draining, it is likely to be infected and in need of medical attention. The same goes for swollen nodes in the armpits, neck, or groin, and if you have a fever or chills.
Impetigo
This condition is caused by a bacterial infection that produces crusty skin lesions that itch first and ooze later. A doctor often can diagnose impetigo simply by looking at it.
Antibacterial creams are an effective treatment for mild infections, but more severe cases require oral antibiotics. The lesions seldom leave scars, even though they are slow to heal. Prevent the spread of impetigo by using clean washcloths and towels, and do not share towels, clothing, razors, or any similar items with friends or family members.
Lichen Simplex
This very itchy patch of skin develops after repetitive scratching and rubbing. The itch could be there because of any one of several skin conditions, including psoriasis, eczema, a fungal infection, or an insect bite. Other symptoms are a leathery or scaly texture of the affected areas, or a raised patch of skin that is red or darker than the rest of your skin.
Women are more likely to develop lichen simplex than men. It usually occurs between the ages of 30 and 50.
The condition is not contagious and usually affects just one side of the body, but the itching is so bad it can interrupt sleep and affect quality of life. The areas most often affected are the head, back of the scalp, neck, lower legs, wrists, forearms, ankles, and genitals. Anxiety and stress can trigger the itching.
Treatment options are topical steroids, steroid injections, moisturizers, cooling creams that contain menthol, and antihistamine or antidepressant medications to help you sleep.
Lupus
Lupus is a chronic disease in which the body’s immune system attacks its own healthy cells, tissues, and organs by mistake. There are four types of lupus, but the most common and serious form is systemic lupus erythematosus, which can affect many parts of the body, including the skin. Other potential targets are the joints, lungs, kidneys, and blood.
Lupus can affect anyone at any age, but women get it more often than men. It is typically diagnosed between ages 15 and 45 and is more common in Asians and African Americans than in other ethnic groups.
Butterfly Rash
A “butterfly rash” is at the top of the list of symptoms. It is a reddish eruption across the bridge of the nose and cheeks. Other symptoms of lupus include fever, fatigue, and weight loss; a rash in an area exposed to sunlight; raised, scaly patches; arthritis involving multiple joints for several weeks; mouth or nose ulcers; kidney problems (detected with blood tests); anemia, low blood cell count, or low platelet counts; and seizures.
Because the symptoms vary from person to person, lupus is difficult to diagnose. There is no single test that can absolutely confirm that a person has lupus. Instead, your physician (or a rheumatologist) will compile a comprehensive medical history, conduct a physical exam, and put you through a battery of laboratory tests.
Treatments
If and when lupus is diagnosed, treatment includes rest, exercise, physical therapy, and medications—nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, antimalarial drugs, and medications that suppress the immune system. It is important for a person who has lupus to avoid exposure to sunlight and UV rays emitted indoors by fluorescent and halogen lights.
In Chapter 5
The next chapter covers skin conditions from Lyme disease to wrinkles and what you can do about them.
The post 4. Skin Conditions: From Acne to Lupus appeared first on University Health News.
Read Original Article: 4. Skin Conditions: From Acne to Lupus »