Diagnosing Diabetes Is a Critical First Step
Many people have diabetes but don’t know it—it’s estimated that as many as 7.2 million people with diabetes haven’t been diagnosed. One reason for this is that symptoms are rare in the early stages of diabetes, so people simply aren’t aware that their health is compromised. However, diabetes is a very dangerous disease, and the sooner it is diagnosed, the sooner you can take steps to prevent possible complications.
Dangers of Diabetes
Diabetes can cause serious complications, including nerve damage in your limbs (particularly in your feet and legs), kidney disease, heart attack, stroke, and blindness.
People who have diabetes are at increased risk of heart disease because diabetes damages your blood vessels, as well as the nerves that control your blood vessels and your heart. People with diabetes have nearly double the risk of dying from heart disease or stroke as people without diabetes.
“Diabetes is the ‘perfect storm’ for heart disease since it causes or contributes to several risk factors, including elevated blood lipids, chronic inflammation, damage to small and large blood vessels, and chronic metabolic stress,” explains Melissa Katz, MD, an assistant professor of clinical medicine at Weill Cornell Medicine.
WHAT YOU SHOULD KNOW
You’re at risk for prediabetes and type 2 diabetes if you:
- Are overweight or obese
- Are age 45 or older
- Are physically active less than three times a week
- Have a family history of diabetes
- Have a history of gestational diabetes while pregnant
- Are age 19 to 44, are overweight or obese, and have one or more other risk factors.
Diabetes Tests
“Testing is appropriate for people with obesity, coronary artery disease, a family history of diabetes, hypertension (high blood pressure), and hyperlipidemia (a high level of fat in the blood),” says Dr. Katz.
The U.S. Preventive Services Task Force recommends blood glucose screening for adults aged 40 to 70 years who are overweight or obese, and advises that screening should be considered for people who are younger and have a lower body mass index if they have risk factors for diabetes (see “What You Should Know” for risk
factors).
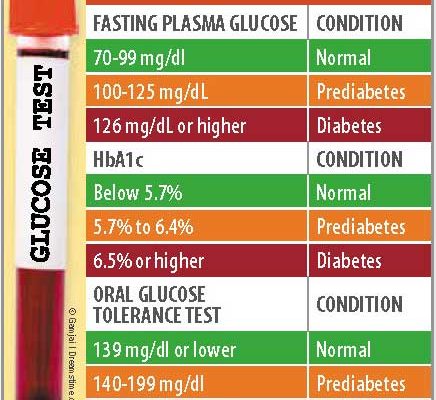
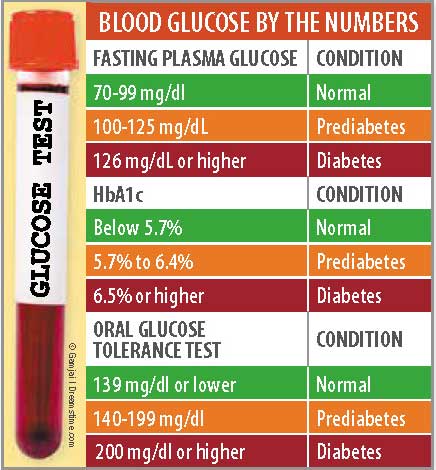
There are three screening tests commonly used for diabetes:
▶ A fasting plasma glucose (FPG) test; fasting is required for at least eight hours prior to the test.
▶ An oral glucose tolerance test (OGTT). This test measures your blood glucose before and after you drink a beverage that contains glucose.
▶ An HgbA1c (also referred to as “A1c”). The A1c measures average blood glucose for the past two to three months, and no fasting is required prior to testing.
Diabetes Medications
Type 2 diabetes medications are designed to regulate the way the body metabolizes glucose (sugar). There are six classes of diabetes medications that work in different ways. In recent years, researchers have identified new mechanisms that can be used to decrease glucose levels; these discoveries have led to the development of many new medications.
“Medication selections should be individualized for each patient,” says Dr. Katz. “Issues to be considered when choosing the appropriate therapy for a particular woman include her age, weight, kidney function, risks and possible side effects associated with each type of drug, and the mode of administration.” For example, some medications come in pill form, while others are administered via injection.
Your doctor also needs information about your lifestyle, including how much you exercise, your eating habits, how often you miss medication doses, and how often you check your blood glucose level to determine which medication is best for you.
Sometimes, more than one diabetes drug is needed to achieve adequate blood glucose control.
Diet and Exercise
Along with medication, diet and exercise are critical components of diabetes treatment.
What you eat has a significant impact on how your body manages insulin. Since foods that contain carbohydrates are broken down into glucose, controlling the amount and type of carbs you eat is key for controllling blood glucose levels.
If you need help with your diet, see a registered dietitian nutritionist who is a certified diabetes educator (CDE), who can explain which foods and eating habits will aid with blood glucose control.
Exercise improves how your body responds to insulin, which, in turn, improves blood glucose control. For help with exercise, consult a physical therapist or other exercise expert who can create an exercise program that is safe and effective for you.
Prevention
If you’ve been diagnosed with prediabetes—a fasting blood glucose level between 100 and 125 mg/dL—you need to take action to prevent diabetes. One resource that may help is the National Diabetes Prevention Program (DPP), which was developed by the U.S. Centers for Disease Control and Prevention. The program includes six months of weekly sessions with a lifestyle coach, followed by monthly sessions.
The DPP covers stress reduction, dietary coaching, and strategies to increase moderate physical activity. A specially trained lifestyle coach will help you set individualized weight-loss and exercise goals and provide educational materials and support to help you reach those goals. To find a DPP in your area or to learn more about the DPP, check out www.cdc.gov/diabetes/prevention. Online, teleconferencing, and Skype options have been added to increase access to the DPP. There are also many non-profit groups and doctors’ offices that offer diabetes support groups and education.
The post Diagnosing Diabetes Is a Critical First Step appeared first on University Health News.
Read Original Article: Diagnosing Diabetes Is a Critical First Step »
Powered by WPeMatico