A Guide to Osteoporosis Medications
According to research published online January 1, 2014 in the New England Journal of Medicine, a new drug called romosozumab may offer hope for the treatment of osteoporosis. The drug works by freeing the body’s ability to stimulate bone production by blocking signals that naturally inhibit bone formation. According to researchers, all dose levels of romosozumab were associated with significant increases in bone mineral density at the lumbar spine. Romosozumab was also associated with large increases in bone mineral density at the total hip and femoral neck. Aside from mild, generally nonrecurring injection-site reactions, the side effects of the drug were minimal.
Current treatment options
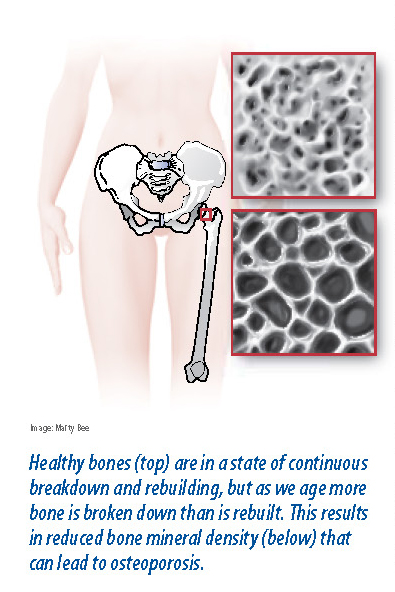
 Bisphosphonates are currently the most common drug prescribed for osteoporo-sis. Bisphosphonates are anti-resorptive drugs, interfering with the natural process that results in the breakdown of bone. Bone is growing tissue: Through our lifetime, old bone is broken down (resorption) and new bone is formed. In our youth, more bone is formed than is broken down, but after about age 30, bone resorption begins to exceed bone formation. This discrepancy speeds up after menopause, and can cause a loss of bone mass that leads to osteoporosis, in which the bones become less dense and more prone to fractures. Bisphosphonates im-pede bone resorption by interfering with the ability of osteoclasts, the cells that break down old bone, to bind to bone.
Bisphosphonates are currently the most common drug prescribed for osteoporo-sis. Bisphosphonates are anti-resorptive drugs, interfering with the natural process that results in the breakdown of bone. Bone is growing tissue: Through our lifetime, old bone is broken down (resorption) and new bone is formed. In our youth, more bone is formed than is broken down, but after about age 30, bone resorption begins to exceed bone formation. This discrepancy speeds up after menopause, and can cause a loss of bone mass that leads to osteoporosis, in which the bones become less dense and more prone to fractures. Bisphosphonates im-pede bone resorption by interfering with the ability of osteoclasts, the cells that break down old bone, to bind to bone.
“Bisphosphonates are all very effective in reducing fracture risk by about 40 percent,” says Zhaoping Li, MD, a physician at UCLA Health System. “Alendronate, the first FDA approved bisphosphonate for use in the United States, is now generic making it the most affordable treatment of the prescription pharmacologic agents available for treating osteoporosis.”
There are several different kinds of bisphosphonates available, as well as other classes of drugs that help treat bone loss.
Oral bisphosphonates—alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva)—are often the first-line treatments for osteoporosis. Research has shown that Fosamax and Actonel may slow the rate of bone thinning and produce modest increases in bone mass.
Fosamax and Actonel are the only oral bisphosphonates approved for use in both men and women. Boniva also is administered as an intravenous injection, as is another bisphosphonate, zoledronic acid (Reclast).
You must take the medication first thing in the morning with a full glass of water in a sitting or standing position, and wait at least a half-hour before lying down, eating, or taking any other drugs or supplements.
The drugs tend to be well tolerated and the most common side effects are gastrointestinal problems. “Major side effects of bisphosphonates can include: 1) esophageal irritation, with some reports linking their use to esophageal cancer; 2) osteonecrosis (cancer) of the jaw; 3) atrial fibrillation (particularly with the IV form, zolendronic acid),” says Dr. Li. “Even with these stated risks, when one is concerned about fracture prevention in patients who are at high risk, the balance is still in favor of using bisphosphonate therapy.”
Bisphosphonate alternatives
 Teriparatide (Forteo), a synthetic version of human parathyroid hormone, can slow bone loss and stimulate bone growth to a greater degree than bisphosphonates. Typically reserved for men and women with more severe osteoporosis or those who’ve suffered fractures while using a bisphosphonate, Forteo is administered as a daily self-injection and can’t be used for more than two years. Af-terward, patients often need bisphosphonate therapy to maintain the gains in bone density from Forteo.
Teriparatide (Forteo), a synthetic version of human parathyroid hormone, can slow bone loss and stimulate bone growth to a greater degree than bisphosphonates. Typically reserved for men and women with more severe osteoporosis or those who’ve suffered fractures while using a bisphosphonate, Forteo is administered as a daily self-injection and can’t be used for more than two years. Af-terward, patients often need bisphosphonate therapy to maintain the gains in bone density from Forteo.
The treatment may raise calcium levels. Your doctor may not recommend Forteo if you’ve undergone radiotherapy of your bones or have Paget’s disease, both of which increase your risk of a type of bone cancer (osteosarcoma).
Calcitonin (Calcimar, Miacalcin), a natural hormone given as a nasal spray, may help relieve pain from spinal compression fractures, but is not very effective at preventing fractures, and plays a limited role in osteoporosis treatment. It may be used in certain men and women who can’t tolerate other osteoporosis medications.
Raloxifene (Evista) slows bone thinning and may slightly increase bone thickness. Used only in postmenopausal women, Evista also may reduce the risk of certain breast cancers, however it can increase the risk of a blood clot in the legs or lungs. The drug may be a reasonable choice in individuals who cannot take a bisphosphonate or who may receive benefit from some of the other effects of the medication.
Estrogen, administered as a daily pill or adhesive patch, has been shown to slow bone thinning and reduce hip fracture risk in postmenopausal women. However, after the Women’s Health Initiative study in 2002 found that supplemental estrogen increased a woman’s risk of heart disease and breast cancer, blood clots, and gall bladder disease, many physicians do not use it solely to treat osteoporosis. Estrogen may be used when other postmenopausal symptoms are present, but only at the lowest dose and shortest duration possible.
The post A Guide to Osteoporosis Medications appeared first on University Health News.
Read Original Article: A Guide to Osteoporosis Medications »
Powered by WPeMatico


