1. Getting a Better Picture of Your Brain
The BRAIN Initiative
Never before has so much science been focused on exploring the secrets of the human brain. In October 2015, the National Institutes of Health announced a second wave of grants to support the Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative, bringing the NIH’s annual investment to $85 million, in addition to $46 million invested the previous year. The funding at 125 institutions in the United States and eight other countries will expand NIH’s efforts to develop new tools and technologies to understand the functions of neural circuits and capture a dynamic view of the brain in action.
The BRAIN Initiative was launched by President Obama in 2014 as a large-scale effort to equip researchers with fundamental insights necessary for treating a wide variety of brain disorders, including Alzheimer’s disease. The goal is to catalyze new treatments and cures for devastating brain disorders and diseases that are estimated by the World Health Organization to affect more than 1 billion people worldwide.
Even before the BRAIN Initiative, the National Institute of Neurological Disorders and Stroke estimated that scientists have learned more about the brain in the last decade than in all the previous centuries. The accelerating pace of research in neurological and behavioral science and the development of new research techniques mean we know more than ever before about the brain.
Protecting Your Aging Brain
What might these breakthroughs mean for your brain as you get older? Experts believe that improved understanding of the brain, coupled with a population better informed about health and nutrition, can help reduce the toll of Alzheimer’s disease and other forms of dementia.
One British study, for example, reported that dementia rates among people 65 and older have actually dropped sharply over the past two decades. In Denmark, another study found that people now in their 90s scored substantially higher on a standard test of mental ability than 90-year-olds did a decade before. Evidence also shows that people who take steps to control their blood pressure and cholesterol have a lower incidence of dementia.
Other research suggests that it’s never too early to start taking better care of your brain. A 2015 study published in the journal Brain reported that the changes in the brain associated with Alzheimer’s disease may be detectable years before the onset of the disease, even in people as young as 20. The findings suggest that Alzheimer’s disease is truly a lifelong process and that preventive interventions may need to begin much earlier.
You Can Make a Difference
Memory loss and other signs of cognitive decline are not inevitable. It’s true, however, that occasional lapses in memory occur more frequently as people get older. But the serious cognitive losses associated with Alzheimer’s disease and other types of dementia are not natural parts of aging. Forgetting where you put your car keys or slipping on a person’s name is normal; putting your keys in the stove or being unable to recognize your grandchildren is not.
While some risk factors for Alzheimer’s and other forms of dementia, such as genetics, are beyond your control, the good news is that there is much you can do to preserve and even improve your “brain power.”
Your Three-Pound Miracle
When you consider all that the human brain does, it seems miraculous that it weighs only about three pounds. But those are an amazingly hard-working three pounds, carrying on thousands of chemical reactions every second. As a result, although on average the brain makes up only two percent of a person’s body weight, it consumes 20 percent of the oxygen you breathe and 20 percent of the energy you take in from food.
To understand how the brain works, think of it like a team composed of specialized players (see Box 1-1, “The Brain”). The hindbrain, which includes the upper spinal cord, brainstem and cerebellum, controls the body’s vital functions, such as heart rate and breathing. The cerebellum also manages movement and the actions your body has “memorized,” such as swinging a golf club or playing the piano. The midbrain, the uppermost part of the brainstem, controls some of your reflexes and is part of the process that coordinates eye movements and other voluntary motions.
Meet the “Thinker”
Those activities we broadly call “thinking” take place in the cerebrum, part of the forebrain, located at the top of the brain. When you read a novel, play chess, compose an email or recognize a loved one’s face, your cerebrum is at work. It stores your memories and enables you to plan and carry out those plans—what cognitive scientists call “executive function.”
What about your “left brain” and “right brain”? These terms refer to the cerebrum’s two hemispheres. Each hemisphere specializes in certain kinds of tasks the brain performs: Typically, the right side of the brain is responsible for more “creative” functions, while the left hemisphere performs grammar, vocabulary, and “logical” functions. Both hemispheres actually contribute to many of these processes, however.
Each hemisphere also controls the opposite side of the body, with nerve signals crisscrossing between the brain’s right hemisphere and your left hand, and vice versa. So when one side of the brain is damaged, such as by a stroke or traumatic injury, it’s the opposite side of the face and body that may droop or be paralyzed.
Specialized Lobes
Parts of the brain called “lobes” handle specific tasks. The frontal lobes, located behind the forehead, take charge of planning, weighing alternatives, and envisioning possible consequences. One way they seem to do this is by temporarily storing options and thoughts you are considering (“Pizza tonight … or Chinese?”) in “working memory.” Some of the research findings about protecting your brain relate specifically to this process.
At the back of each frontal lobe, a motor area helps manage voluntary movement. Nearby, on the left frontal lobe, Broca’s area is responsible for turning your thoughts into words.
The parietal lobes, located behind the frontal lobes, handle sensory input and are also important for math and reading. The occipital lobes at the back of the brain process images from the eyes. Under the parietal and frontal lobes, the temporal lobes perform similar chores with input from the ears, as well as integrating sensory information and memories.
Going Deeper
Several structures in the interior of the brain act as mediators between the cerebral hemispheres and the spinal cord; these include the thalamus and basal ganglia. The hypothalamus, also in the interior of the brain, is important for maintaining your sleep/wake cycle, food and water intakes, and responses to stress.
Important to your brain, but far out of proportion to its size, the tiny hippocampus acts as a sort of hard drive for your memories. It “indexes” your memories and sends them to other parts of the brain when needed.
The Brain’s “Bark”
When you hear about the “gray matter” of the brain, that’s referring to the coating of the surface of the cerebrum and cerebellum, about an eighth of an inch thick —sort of like the bark on a tree. Formally called the cerebral cortex—from the Latin for “bark”—it really is gray. That’s because the cortex lacks a white insulating material called myelin that is found elsewhere in the brain; this myelin sheath allows electrical impulses to transmit quickly and efficiently along nerve cells. Myelin makes most of the brain white, so you will also see references to “white matter.” The cortex also is famously wrinkled, and these folds serve a purpose: Much of the brain’s information processing occurs in the cerebral cortex, and its wrinkles create more surface area for this processing.
Networks of Nerves
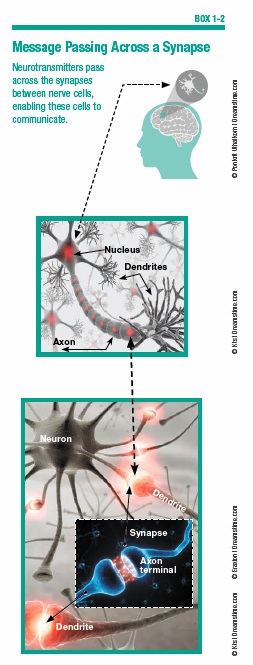
That’s the big picture of your brain. Zooming in to the microscopic level, thinking and other functions of the brain and nervous system are performed by cells called neurons (see Box 1-2, “Message Passing Across a Synapse”). An adult brain contains approximately 100 billion neurons, with branches that connect at more than 100 trillion junction points called synapses.
Neurons consist of several parts: the cell body, which includes the nucleus and most of the molecules that keep the neuron alive; dendrites, which act like telegraph wires bringing data from other neurons; and axons, which carry the signals away to other cells in the body. Neurons transmit signals via synapses using special chemicals known as neurotransmitters.
Malfunctions of these neurotransmitters are associated with certain diseases of the brain. For example, a characteristic feature of Alzheimer’s disease is a reduction in levels of acetylcholine, a neurotransmitter involved in memory. Parkinson’s disease is linked to low levels of dopamine, a neurotransmitter important in controlling movement.
Your Plastic Brain
A common misperception is that neurons form new connections only during early brain development. In fact, even adult brains can form new neuronal connections, strengthen existing ones, or eliminate old ones as you continue to gather new knowledge and experiences. This ability of the brain to change in response to new inputs is called plasticity. Stimulating neurons can cause them to grow and form new synaptic connections, while those that go without stimulation may weaken.
This plasticity helps explain why practicing a task, such as learning to play a musical instrument, helps a person perform that task better and more efficiently. Doing something over and over again strengthens the synapses involved in that task—like paving a road to make repeated journeys go more smoothly.
The Other 90 Percent
You may have heard another misconception—that humans “use only 10 percent of our brains.” That myth may have originated in the fact that glial cells, smaller but more numerous than neurons, make up about 90 percent of the cells in your brain. Until recently, scientists viewed glial cells as little more than packing material around the neurons.
Now, however, experts believe glial cells are part of an important system that removes toxic material and waste products from the brain. The “trash” that glial cells help take out can include the beta-amyloid proteins that clump together to form plaques in Alzheimer’s disease. Glial cells might also work to destroy dangerous neurons that excrete too much beta-amyloid.
Glial cells also supply nerve fibers with energy, and may assist neurons with information processing and signaling. Chronic disease, inflammation, and stress can harm glial cells, while healthy nutrition and regular exercise are believed to benefit glial cells much as they do other parts of the brain.
What Can Go Wrong
When things go wrong in the brain, there can be symptoms of a decline in cognition—what we loosely call thinking and memory—that affect a person’s ability to conduct everyday activities. The umbrella term for a wide range of such symptoms is “dementia,” which is not a specific disease or single condition. The best-known form of dementia, Alzheimer’s disease, accounts for 60 to 80 percent of all cases.
The earliest signs of dementia may be what’s called mild cognitive impairment (MCI), a stage between normal forgetfulness due to aging and more serious cognitive decline (see Box 1-3, “Symptoms of Mild Cognitive Impairment”). Mild cognitive impairment manifests as problems with thinking and memory that do not interfere with everyday activities. People with this condition are often aware that they are showing signs of impairment. Not everyone who develops mild cognitive impairment progresses to Alzheimer’s or other dementia.
Progression to Dementia
Many of the first symptoms of actual dementia are common in everyday life for people who are perfectly normal, such as being unable to come up with a word that’s on the tip of your tongue or misplacing things (see Box 1-4, “Early Signs of Dementia”). Many of these early signs of actual dementia are also similar to the symptoms of mild cognitive impairment. To be considered dementia, at least two of these core mental functions must be significantly impaired:
- Ability to focus, pay attention
- Communication, language
- Memory
- Reasoning and judgment
- Visual perception
As dementia becomes worse, symptoms grow more obvious and interfere with the ability to take care of oneself and conduct everyday life. People with severe dementia may no longer be able to perform basic activities of daily living, recognize family members, or even understand language.
The Brain Changes of Alzheimer’s
Unlike dementia in general, Alzheimer’s disease is associated with specific changes in the physical condition of the brain. A brain affected by Alzheimer’s has far fewer nerve cells and synapses than a healthy brain. The “gray matter” actually begins to shrivel, impairing the ability to process information. The hippocampus, so important to the formation of new memories, shrinks. Fluid-filled spaces within the brain, called ventricles, grow larger.
Characteristic Formations
When reading about Alzheimer’s disease, you’ll see references to two types of characteristic brain formations, called plaque and tangles. Plaque is formed when pieces of a “sticky” protein called beta-amyloid, which comes from fatty membranes that surround nerve cells, clump together. Scientists suspect that bigger plaques may not be as damaging to brain function as smaller clumps of beta-amyloid that block the messaging between the brain’s synapses.
Tangles are like traffic jams in your brain. In a healthy brain, parallel strands of “tau” proteins function like highways, carrying essential nutrients. In Alzheimer’s patients, tangles of collapsed tau block the orderly flow along the highways that serve the brain. Eventually, the cells deprived of nutrients die.
As these plaques and tangles spread through the “gray matter” of the brain, Alzheimer’s disease progresses. Typically, plaques and tangles strike first in areas important to learning, memory, thinking, and planning.
Diagnosing Disease
The earliest stages of Alzheimer’s may begin as many as 20 years before the disease is severe enough to be diagnosed. When Alzheimer’s strikes relatively younger people, it may not be characterized by the memory problems we associate with the disease (see Box 1-5, “Alzheimer’s Doesn’t Always Start with Memory”).
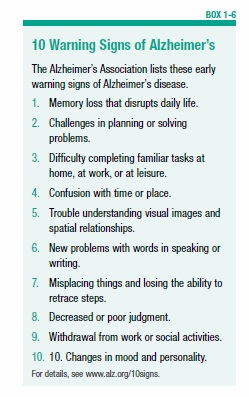
In mild and moderate stages of Alzheimer’s, the growing plaques and tangles impair mental functions enough to affect everyday activities and to be noticed by loved ones. This is when the disease is most often diagnosed (see Box 1-6, “10 Warning Signs of Alzheimer’s”).
People with Alzheimer’s, which is a fatal disease, live an average of eight years after diagnosis, but some survive as long as 20 years.
Brain Pictures
At one time, the diagnosis of Alzheimer’s disease could be definitively confirmed only after death, via autopsy. But today, new imaging techniques make it possible to see the damage the disease causes in a living brain and to better understand how healthy brains function.
You may have even undergone some of these scans yourself, for other parts of your body, such as the CT scan. Short for “computed tomography,” these computer-assisted scans assemble a static cross-section of the brain using X-rays.
More detailed pictures of the brain, without the use of X-rays, can be obtained by magnetic resonance imaging (MRI). This technology takes advantage of the fact that hydrogen atoms in the brain can be affected by rotating a powerful magnet around a person’s head; the resulting changes in these atoms’ energy levels can be captured to create detailed images. Both CT and MRI scans are static—like snapshots of the brain.
Brain Movies
To create images of the brain in action—like movies or videos—scientists employ fMRI scans, short for “functional magnetic resonance imaging.” These scans track the movement of oxygen-carrying hemoglobin—the protein in red blood cells. Because these look different from hemoglobin not carrying oxygen, active areas appear lighter, creating a moving image of the blood flow in the brain.
Another functional imaging technique is the PET scan, an acronym for “positron emission tomography.” PET scans track special molecules that are tagged with a radioactive substance. Because patients can be awake and engaged in mental tasks while undergoing PET scanning, this technology can monitor changes in the activity of the brain as it works.
The Heart-Brain Connection
Every heartbeat carries roughly one-fifth to one-quarter of your blood supply to the brain, and an even greater percentage when your brain is working hard. The brain is fed by one of the richest networks of blood vessels in the body, so changes in your cardiovascular system affect brain function. That means many of the ways in which you can protect your brain also benefit your heart, and vice versa, because a healthy brain depends on a healthy cardiovascular system.
The second-most common form of dementia after Alzheimer’s disease, in fact, begins with blood vessel damage in the brain. In vascular dementia, a stroke or a series of tiny strokes cuts off or restricts the flow of blood to brain cells, interfering with their ability to communicate with other brain cells. That in turn affects everything from your ability to think to your emotions. Vascular dementia may manifest in different ways depending on which areas of the brain suffer damage.
Blood-vessel changes can also increase the degree of impairment or the speed of cognitive decline in other forms of dementia, such as Alzheimer’s, or a condition known as dementia with Lewy bodies.
Recent research has even suggested that a healthy heart and blood pressure in midlife might be associated with brain volume decades later (see Box 1-7, “Cardiovascular Fitness Now Linked to Brain Volume Later”). It could also be that the association goes the other way, and a healthy brain contributes to cardiovascular health.
Protecting Your Heart and Brain
This heart-brain connection means that, although some risk factors for Alzheimer’s and other dementias you can’t control, others you can. In particular, you can help protect your brain by improving your cardiovascular health with these steps:
- Keep your blood-cholesterol levels healthy by cutting down on saturated and trans fats and, if prescribed by your doctor, taking cholesterol-lowering drugs, such as statins.
- Replace unhealthy fats with unsaturated fats; current evidence suggests that polyunsaturated fats, found in liquid vegetable oils and nuts, are the most heart-healthy choice, though other benefits have been associated with monounsaturated fats, found in olive and canola oils and avocados.
- Control your blood pressure by reducing salt intake, following a healthy diet (the DASH eating plan is specially formulated to combat hypertension—see 1.usa.gov/1n6HQFI to learn more), and taking blood-pressure medications if prescribed by your doctor.
- If you smoke, here’s another reason to quit; and if you don’t smoke, don’t start.
- Follow a heart-healthy diet, such as DASH (see above) or a Mediterranean-style diet, which we’ll explore in the next chapter.
- Maintain a healthy weight.
- Maintain healthy blood-glucose levels by watching your weight and reducing intake of refined carbohydrates, starches, and sugar to avoid diabetes, which in turn contributes to heart disease.
- Follow exercise guidelines, which generally advise getting 30 minutes a day of at least moderate physical activity on most days of the week. Exercise seems to directly benefit brain health by increasing blood and oxygen flow to brain cells, and benefits your overall cardiovascular system.
As we’ll see in the rest of this Special Health Report, smart choices about nutrition and lifestyle can make a big difference. Your brain is the hardest-working three pounds of your entire body, so it’s important to do everything you can to make sure it lasts a lifetime.
The post 1. Getting a Better Picture of Your Brain appeared first on University Health News.
Read Original Article: 1. Getting a Better Picture of Your Brain »
Powered by WPeMatico